Tunnelled Haemodialysis Catheter
This leaflet outlines the process of having a tunnelled haemodialysis catheter inserted. It has been given to you to supplement the information already provided by your doctor or nurse.
What is a tunnelled haemodialysis catheter?
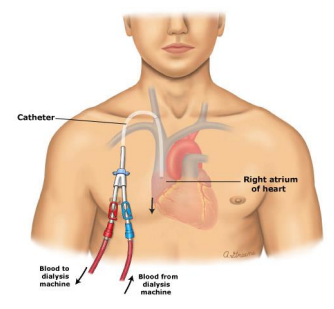
A haemodialysis catheter, or ‘line’, is a tube roughly twice the length and half the width of a pen, which is inserted into one of your larger veins. It provides access to your blood stream to allow blood to be ‘cleaned’ by a dialysis machine.
There are two types of dialysis catheter: a tunnelled catheter and a temporary catheter.
Tunnelled catheters are typically placed into a vein in the neck but can also be inserted in the groin. The catheter passes under the skin between the neck and chest wall (through a tunnel) so that it comes out on the skin below the collarbone. It is held in place by a ‘cuff’ under the skin.
Tunnelled catheters are inserted when it is likely they will be needed for several weeks and are more comfortable and less likely to develop infection than temporary lines, which usually only remain in place for a maximum of three weeks.
What is haemodialysis and how is the catheter used?
Healthy kidneys work by filtering blood and removing excess fluid from the body in the form of urine. When your kidneys do not function properly and they are unable to do this as well, fluid and toxins build up in the body. Your consultant will have diagnosed kidney failure and have suggested haemodialysis is needed, which will require a dialysis catheter.
In order to carry out haemodialysis, nurses access your blood stream via a catheter with two ends, or lumens. Blood is removed via the red catheter/ arterial lumen, passed through the dialysis machine tubing by the action of a pump, into an artificial kidney. Here your blood is filtered, toxins and fluid are removed, and the ‘clean’ blood is returned back to the body through the blue/ venous lumen.
The first haemodialysis procedure takes two hours, increasing to four hours within the first few sessions. Eventually you will be receiving these four hour dialysis treatments three times per week on alternate days.
How do I prepare for the dialysis catheter insertion procedure?
You may eat and drink normally on the day of the procedure, unless you have been told otherwise. You will be advised to shower on the morning of the procedure, and will be asked to use an antimicrobial wash lotion called Octenisan®. This is to minimise the risk of infection. You will be given instructions on how to use this, please follow them carefully.
You will have a clotting blood test done beforehand (please inform your nurse or doctor if you are on any blood thinning tablets such as Warfarin, Clopidogrel or Aspirin, as these may need to be stopped for some time prior to the procedure).
We must, by law, obtain your written consent to this procedure beforehand. Staff will explain all the risks, benefits and alternatives before asking you to sign a consent form. If you are unsure about any aspect of the treatment proposed, please do not hesitate to speak with a senior member of staff.
Who will carry out the procedure and where?
A renal consultant or specialist registrar will insert the haemodialysis catheter. It will take place in a dedicated procedure room on the Prince of Wales Ward at Dorset County Hospital and you will be accompanied by a member of nursing staff or a second doctor. Occasionally, the procedure may be carried out by a radiologist in the hospital’s X-ray Department.
How long will it take?
The actual procedure usually takes approximately 30 minutes. If you are coming in as an out-patient, please expect to be in the hospital for approximately three hours.
What happens during the procedure?
The insertion of a dialysis catheter is carried out in strict sterile conditions. The doctor will wear a gown and gloves, and you will remain awake throughout the procedure. Prior to the insertion of your catheter, the doctor will ask you to lie flat on a trolley which will be tilted so your head is slightly lower than your feet. The skin on your chest will be cleaned with an antiseptic (ChloraPrep®) and covered by a sterile drape. Please inform your doctor beforehand if you are allergic to any antiseptic products.
An ultrasound probe will be used to identify the correct position of the vein in your neck, which takes blood to the heart. Local anaesthetic is then injected into the skin around this vein. Several injections may be needed. Once the skin is numb, a guidewire is inserted into the vein to help position the catheter properly. Local anaesthetic will then be injected into a different area below your neck, at the top of your chest. This will be the location where the catheter exits your skin. After the guidewire is inserted in the neck, a small incision is then made on your chest, and the catheter is inserted through your neck. The catheter is pushed under the skin for a few centimetres until it meets the guidewire. The catheter is then inserted into the vein over the guidewire, which helps to guide the catheter into place. The ends, or lumens, of the catheter will hang outside of your body through the incision that was made in your chest. You may feel some pressure as the line is being pushed, but you should not feel any pain. Please let the doctor know if you are uncomfortable, and more local anaesthetic may be given. The catheter is initially held in place by stitches to give the skin time to heal around the cuff. Healing usually takes two to three weeks. The stitches in your neck will be removed one week after insertion and the wing stitches on your chest will be removed one month after insertion.
What happens after the catheter has been inserted?
If you have had a neck line inserted, a chest x-ray will be needed before your first dialysis procedure to confirm correct positioning. If the line was inserted in the X-ray Department, then a separate chest X-ray will not be needed.
You may feel some discomfort in the area around the line once the anaesthetic has worn off. Please let your nurse know, as pain relief can be given.
How long will I need dialysis for and what are my other options?
In some cases, haemodialysis is only needed for a short term (days or weeks), such as after a kidney injury, until kidney function recovers. However, for patients with chronic kidney disease there are other treatment options. These include peritoneal dialysis (where waste products are filtered from your blood by using a cleansing fluid that flows through a tube into part of your abdomen); or if you are considered a candidate, there is the option to be put on the transplant waiting list. All of your options can be discussed in more detail with your consultant.
What are the risks of having a dialysis catheter?
The most serious risks associated with the insertion of a dialysis catheter are damage to the vein or a nearby artery causing excessive internal bleeding or puncturing of the lung, but these are extremely rare. Your doctor can explain these risks in more detail with you. Other complications at insertion include:
- Bleeding from the exit site. This can be stopped by applying firm pressure to the exit site and should stop shortly.
- Difficulty placing the line, meaning the doctor will have to stop and discuss having another attempt with you, either on the same day or at a later date.
- Irregular heart rhythm/rate. The doctor will monitor your heart activity during the procedure, but any problems should resolve quickly on their own.
You must contact the renal unit if any of these complications occur after the catheter has been inserted:
- Infection: if you develop high temperature, chills, shivering or sweating. The exit site may appear red and the line may have to be removed to avoid the spread of infection (bacteraemia).
- Difficulty breathing/chest pain: air may have entered the vascular space while on dialysis or at the point of line insertion.
- Catheter dislodgment/complete removal: If the catheter falls out, immediately apply pressure and contact the Prince of Wales Ward.
- Excessive bleeding from the exit site: apply firm pressure immediately. If the bleeding does not stop with pressure applied, contact the renal unit.
- Dressing coming off: do not touch the exit site if the dressing comes off. If you are in hospital, please tell a nurse. If you are at home and have a clean dressing, place it over the exit site and contact the renal unit as you may need antibiotics.
- Stitches break: the catheter is more likely to fall out if the stitches come out before they should. New stitches will need to be inserted.
- Lumen cap comes off: the clamps should be closed with the caps on at all times when the catheter is not in use. This is to avoid blood loss or air entry. The lumen will need to be cleaned and re-capped and antibiotics may be needed.
Be prepared, the nursing staff may ask you to come into your closest renal unit or hospital for treatment if any of these complications occur.
How can I prevent these complications?
- Do not pinch, pull or bend the catheter or use scissors around it.
- It is very important not to get the catheter wet, which can lead to serious infection. Waterproof pouches to cover the line for shower use may be available from your GP by prescription only, however not all GP surgeries supply them. Please speak with your individual surgery to find out about availability.
- Any member of staff using the line must undertake strict infection prevention measures. Please voice your concerns if you do not think this is being done.
- Your catheter should only be used for dialysis. If there is no alternative it can be used to take blood samples by an experienced nurse.
- The catheter must have at least weekly dressing changes. Your skin around the catheter exit site will be cleaned with Chlorhexidine 2%.
If you decide you do not wish to have a tunnelled dialysis inserted and would like to discuss other options for dialysis access or treatment, please speak with your doctor or nursing staff.
If anything unusual occurs, or if you are at all worried or concerned about your dialysis catheter, please contact your Renal Unit. The nurses will be happy to offer advice.
Contacts numbers
Prince of Wales Ward: 01305 255139/ 01305 253316
DCH Dialysis Unit: 01305 255345
Poole Dialysis Unit: 01202 307430
Bournemouth Dialysis Unit: 01202 704411
About this leaflet
Author: Gemma Bickel, Renal Staff Nurse
Written: June 2017
Approved: May 2018
Review date: May 2021
Edition: v1
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet