Risk Reducing Advice – Breast
This advice leaflet will provide information to help you decrease the risk of developing lymphoedema (swelling). Although most lymphoedemas develop in the first few years following surgery/treatment, there is a small lifelong risk so the guidelines should always be followed.
What is lymphoedema?
Lymphoedema is a persistent swelling of any part of your body but after breast cancer surgery/treatment, it commonly occurs in the arms and hands. Swelling can also affect the breast, chest, shoulder or the area on the back behind the armpit. One, some or all of the lymph nodes under the arm can be removed during breast surgery to check whether any cancer cells are present. The lymph nodes and vessels that have been damaged or removed are not replaced, so the lymphatic drainage routes are reduced or altered – this can cause the fluid to build up in the surrounding tissues. About one in five women having breast cancer treatment will have some swelling. It usually starts slowly and is easier to treat when it is mild. If left untreated more swelling, heaviness, leaking fluid, wounds and cellulitis can occur.
The swelling is a collection of fluid within the tissues under the skin which cannot be drained by a needle. This fluid known as lymph is colourless and odourless but it is rich in protein. The high protein content of this fluid causes dryness of the skin which can result in flaking, thickening and blistering.
Why are you at risk of developing lymphoedema?
This may be because you have recently had surgery or treatment where lymph nodes have been removed or treated with radiotherapy or had an infection. The lymph nodes and vessels that have been damaged or removed cannot be replaced, so the lymphatic drainage routes are reduced or altered and this in turn disrupts normal lymphatic flow.
When does lymphoedema occur?
Lymphoedema usually develops in the first two years post-surgery or radiotherapy but it can occur many years later. Therefore there is a lifetime risk of developing lymphoedema following breast cancer treatment where the lymph nodes have been removed or damaged.
Is lymphoedema curable?
Lymphoedema is a long-term condition, which means that once it has developed it can be controlled but is unlikely to ever go away. The symptoms of lymphoedema usually respond well to treatment and this means that in most cases it can be controlled.
How can I reduce my risk of lymphoedema?
It is still not known what exactly causes lymphoedema but the following may help to reduce your risk of developing it.
Weight management
Gaining weight and being overweight is the biggest risk factor in developing lymphoedema. There is strong evidence to suggest that being overweight can increase your risk of developing lymphoedema. It is important to maintain a healthy weight by eating healthily and regular exercise. If you are unsure what a healthy weight is for you, you should ask your health care professional for advice.
Movement and exercise
Gentle movement, exercise and activities will help the muscles pump lymph fluid more effectively through your body. It helps to improve and maintain flexibility and keeps your bones strong. Being more active helps you achieve and maintain a healthy weight and it may improve your emotional wellbeing.
Activities such as walking are ideal as are swimming, cycling, Nordic walking, bowling, gardening, housework and even shopping. Basically, move your body more. Physical activities such as walking and swimming may help to reduce the risk of lymphoedema but should be introduced gradually especially if you’re new or returning to exercise. Evidence suggests regular slow arm movements may help to lower your risk of developing lymphoedema. Slow and gentle arm movements can be incorporated into day-to-day activities. For example, housework particularly the action of dusting. It is also important not to rest your hand and arm all week then try to do your housework or exercise in one big blow-out rather than doing a little bit every day and checking how you’re doing as you go along – ‘No boom and bust’ and stop straight away if you notice any pain or swelling.
Pacing yourself is important
If your mobility is limited, you can still move your body. You can lift your arms and legs when in bed or on the chair.
Set yourself personal and achievable goals, sometimes keeping a record of how much activity you do can be beneficial in achieving your goals.
Try to do a little every day and build up to around 30 minutes of activity/exercise, 5 days a week. If you are used to exercising, it is a good idea to go back to what you have been doing – but start gradually and build up on a day-to-day basis. If you go to a gym or exercise class, remember to pace yourself and listen to your body. Discuss your condition with your instructor so that they can adapt the quantity or intensity of exercise you do if necessary.
There are exercise schemes specifically for patients who have had cancer at various leisure centres throughout West Dorset.
There are specific exercise videos available on the breast cancer care web site or Haven.
Reduce infection – look after your skin
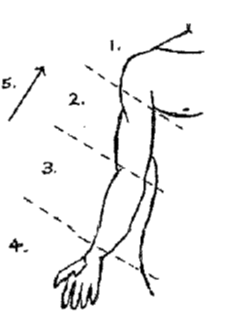
Performing daily skin care can help to reduce the risk of developing an infection and subsequently lymphoedema. Wash your skin daily with warm water and soap. Dry your skin thoroughly especially between your fingers and toes. Apply moisturising cream (not perfumed) to your skin (as the diagram below demonstrates) to prevent it from dryness.
- Gently stroke the skin upwards
- Slow, rhythmical strokes
- Start at top (position 1)
- Work your way down the limb
- Finish by stroking from the and all the way up
- Pat hair back down.
When cutting your nails, take care not to damage the cuticles.
Prevent sunburn by using a high factor sun cream.
Always wear gloves for washing up, gardening and other household tasks.
Use an electric razor or depilatory cream to remove unwanted hair from under your armpits.
Avoid where possible needle-stick procedures such as blood tests, immunisations and tattoos.
Cellulitis signs and symptoms
Skin infections such as cellulitis could cause lymphoedema so it is vital that you check for signs of infection. Symptoms can appear suddenly and make you feel unwell.
Signs of infection can include:
- Swelling of your limb
- Limb feels hot to touch
- Redness or rash on your limb
- Pain
- General feeling of unwell.
If you think you have an infection in your “at risk” arm seek medical help from your GP or the out of hours service. It is important to act quickly to prevent the infection from getting worse. You will need antibiotics and you must take them for no less than two weeks.
Looking after your scar
A scar forms as a result of surgery. Scars are part of the healing process, and we would hope that all are flat, supple and with minimal redness after 12-18 months. During the healing process adhesions can form under the skin and cause tightness, pain increased sensitivity and reduce the flow of lymph fluid.
Scars can be helped by the following advice:
- Try and look at your scar. The surgery may have changed your body and you may need time to adjust to your new body image and how you feel about yourself.
- When your scar has healed, it is important you start to touch and move the scar and the surrounding tissues. Massage the scar in a circular motion with a non-perfumed cream to moisturise the area to keep your skin supple. Focus on the harder, lumpy areas as this will soften and reduce the lump. Touching and massaging the scar will help to reduce adhesions that can form post operatively. It will also reduce tightness and sensitivity and increase movement within the scar and surrounding soft tissues.
Other post-operative symptoms
Nerve disturbance
Numbness, pins and needles, extra sensitivity and stabbing pains are all different forms of nerve irritation that can occur after surgery. The effects of these can be improved by massage and exercise. Sometimes using different textures can alleviate the symptoms i.e. rubbing with a towel then a soft sponge.
Cording and axillary web syndrome
This is a tight band of tissue that looks like pieces of string which can cause restriction of your movement and in most cases is painful or prevents stretching. It is related to the surgery. Stretching exercises can help to relieve these symptoms. Sometimes the cords can snap naturally during activity so do not be alarmed if this happens.
Remember the following three things:
- Reduce or maintain a healthy body weight
- Move your body
- Reduce your risk of an infection.
Contact numbers
We hope that you have found this information useful. If you have any questions or are worried about anything, please speak to the Lymphoedema Department on 01305 255370.
Useful websites
About this leaflet
Authors: Emma Diaz, Lymphoedema Nurse Specialist
Written: May 2018
Updated and approved: July 2025
Review date: July 2028
Edition: v1
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet