Preventing Pressure Ulcers
This leaflet is for patients, parents and carers.
Pressure ulcers – what are they?
When the skin experiences continual or excessive pressure, particularly over a bony area, this can cause a restriction in the blood flow, stopping vital nutrients and oxygen reaching the skin and tissues beneath. If this pressure continues, this can result in damage to the skin that can occur very quickly. This breakdown in the skin is called a pressure ulcer, or a pressure injury.
This can occur from an individual’s own body weight applying pressure or due to a medical or non-medical device (called a ‘device related pressure ulcer’)
What could cause a pressure ulcer?
Children and young people with additional health needs can be at greater risk of developing a pressure ulcer. Take a look at the following factors to pressure ulcer development:
- Exposure to medical devices without routine skin checks: Medical devices may be an important part of your/your child’s daily care; however,
the skin underneath can experience pressure if the device is not rotated or fitted correctly. - Lack of pressure relieving equipment: Sometimes pressure cannot be avoided, but using pressure relieving equipment like
mattresses and dressings can help. - Skin care issues: If you/your child has experienced pressure injuries before, the same area of skin is at greater risk of having further pressure injuries. If you/your child has dry skin issues or the skin becomes hot and humid (like around a ventilator mask) it can be more at risk of breakdown when met with pressure.
- Sitting or lying for long periods of time in the same position: Those who have reduced mobility can struggle to re-position themselves and so cannot reduce the pressure on their skin. Those who cannot verbally communicate can struggle to tell care givers that they are experiencing discomfort from pressure. Those with difficulty experiencing sensation will not reposition themselves if they cannot feel pain.
- Incontinence: Those who are incontinent are more exposed to moisture, and prolonged time in a wet or soiled pad can contribute to pressure injury.
- Poor diet: Without key nutrients the body can struggle to heal.
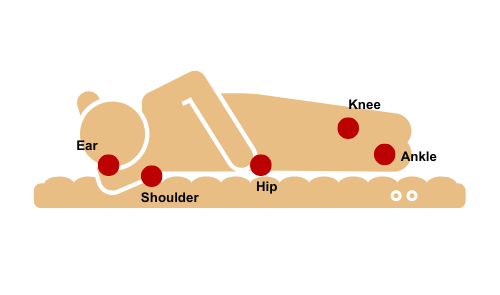
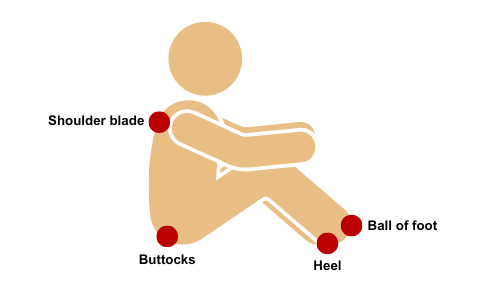
Where can pressure ulcers develop?

What devices can lead to pressure injuries if not monitored?
Ventilator masks
- Oxygen masks
- Oxygen nasal cannulae
- Nasogastric tubes
- Gastrostomy buttons
- Central lines
- Wheelchairs
- AFO boots
These are just a few examples! And remember pressure injuries can also occur from non-medical equipment such as beds and chairs.
What can I look out for as early warning
- Painful areas of skin
- Skin that feels warm to the touch or overly cool to the touch
- Skin that feels boggy and lumpy or hard
- Redness
- Discolouration to usual skin tone
- Purple/blue patches of skin.
What’s so bad about a pressure ulcer?
- Pressure ulcers can be painful and uncomfortable.
- They can lead to more severe skin damage and big wounds in the skin if not treated which can result in infection.
- Treating can result in lost time for the family due to visits from your community nurse, hospital visits, collecting prescriptions etc.
But pressure ulcers can be preventable! So, what can be done to reduce the risk of developing one?
We go by ‘SSKIN’
Here’s what you can do to help at home:
SKIN: Routinely check the skin every day for signs of pressure injury. Check over bony areas. Speak with your community nurse regarding a skin prevention plan. Ensure that after washing your/your child’s skin is dried.
SURFACE: Routinely check that equipment is the right size and fit and if you feel you/your child is growing, call wheelchair services, orthotics, or physiotherapy for a review. Ensure to re-position equipment in contact with the skin routinely.
KEEP MOVING: Ensure your/your child’s position is changed at least every 2 – 4 hours. This is particularly important if they cannot move themselves. Look out for non-verbal cues for pain as this could be pressure.
INCONTINENCE/INCREASED MOISTURE: Ensure you/your child is not sitting in a wet or soiled pad for too long as this could lead to moisture damage, which can contribute to pressure ulcer development. Ensure pads are a suitable size. Speak to your community nurse about barrier creams. Moisture from saliva and gastrostomies can also lead to moisture damage so monitor this skin too.
NUTRITION: Ensure your/your child’s diet is full of protein, and lots of fruit and vegetables. In some instances, your community nurse may refer you to a dietitian for review.
What will your community nurse do to help?
- All children and young people on our caseload are risk assessed for pressure ulcer development. We complete this every year at your annual review, or more frequently depending on you/your child’s need.
- According to this, we then devise a plan to manage you/your child’s pressure ulcer prevention/care.
- We liaise with other professionals to ensure you have appropriate pressure relieving equipment in place if this is required.
If you identify any areas of redness on your child’s skin, please give your community nurse a call and we can talk this through with you.
Contact numbers
We hope that you have found this information useful. If you have any questions, please contact us below:
Team office phone: 01305 254279
Team email address: ccndorchester@dchft.nhs.uk
Address: Community Children’s Nursing Team,
The Children’s Centre
Dorset County Hospital
Dorchester
DT2 9UY
Working hours: Monday to Friday, 9am to 5pm (excluding bank holidays).
Please note: We are NOT an emergency service.
We have an answerphone which is checked twice daily during working hours.
If your contact is urgent, please contact the Paediatric Assessment Unit out of hours on 01305 254218 or Kingfisher Ward 01305 254253.
Useful websites
Wessex Healthier together: what0-18.nhs.uk
Dorset SEND local offer: www.dorsetcouncil.gov.uk/children-families/sen-and-disability-local-offer/dorsets-local-offer
Feedback
If you would like to give us feedback on our Paediatric Community or Specialist Nursing Service, please complete our patient related experience survey: https://dchft.onlinesurveys.ac.uk/paediatric-specialist-and-community-nurses-questionnaire
All responses will be treated anonymously and in the strictest confidence and only used to help us improve our service for patients.
About this leaflet
Author: Beth Maskell, Community Children’s Nurse Specialist Practitioner
Written: October 2023
Approved: December 2023
Review date: December 2024
Edition: v1
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet