Pressure Ulcers
What are pressure ulcers?
Pressure ulcers (bedsores) are areas of damage to skin and underlying tissue. They are usually caused by sitting or lying in one position, without moving, for too long.
A pressure ulcer can develop within a few hours. It usually starts with the skin changing colour – it may appear slightly redder or darker than usual.
Who gets pressure ulcers?
You can be at risk if:
- you are confined to bed or a chair and unable to move yourself independently or have limited movement
- you have loss of sensation or poor circulation
- you have skin that is frequently moist through perspiration or loss of bowel or bladder control
- you have poor nutrition, or you are unwell.
Where do you find pressure ulcers?
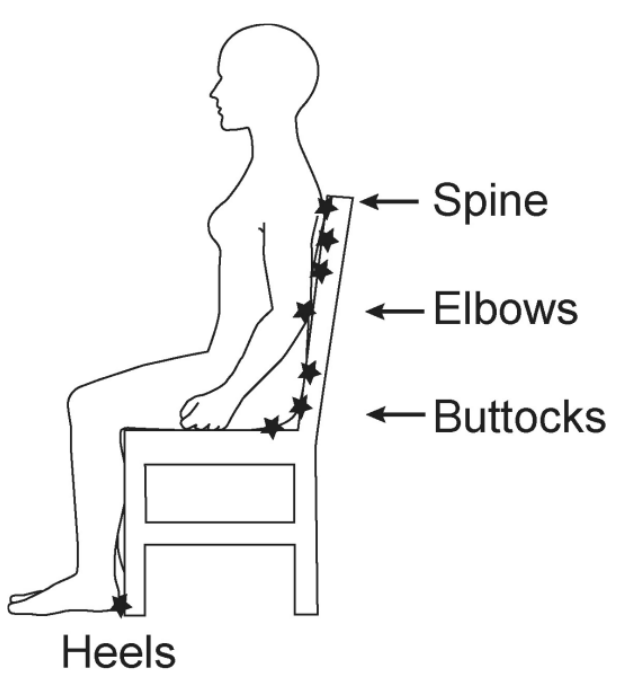
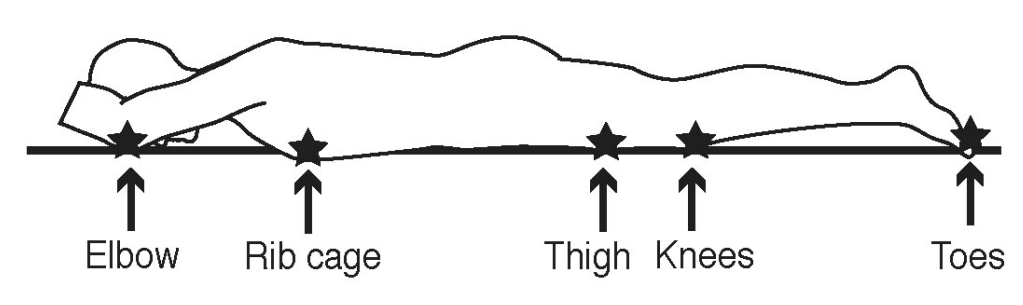
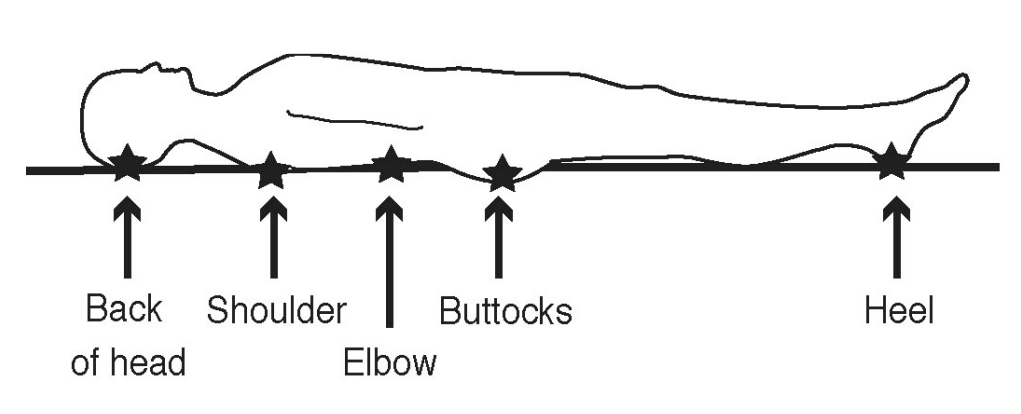
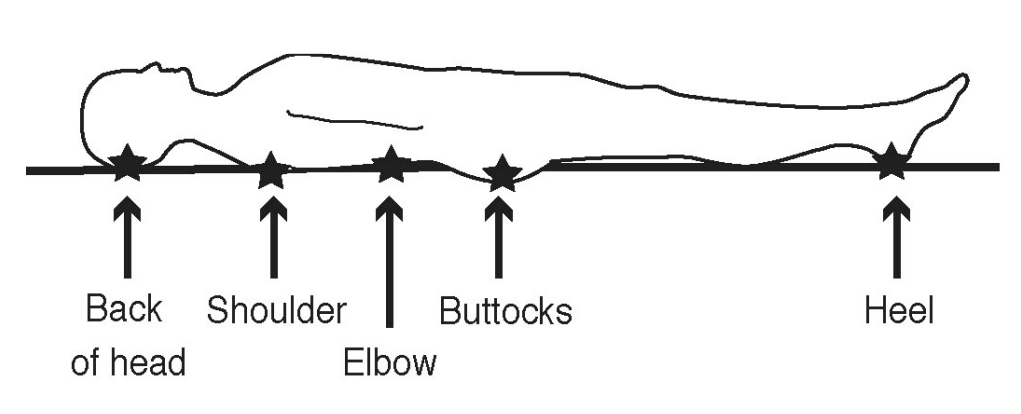
Pressure ulcers occur over areas of the body which support our weight and where bone is near the surface (there is a constant pressure). See diagrams.
Take care of your skin
The aim is to find and correct problems before pressure ulcers form. If you have a problem with perspiration or incontinence, your skin should be cleaned as soon as it gets soiled using a soft cloth or sponge to reduce injury to the skin. Pat dry and apply prescribed barrier cream as directed by your nurse or doctor.
How to help yourself
Check your skin at least once a day in the areas where there is constant pressure. This can be done by your carer, or you can do it yourself; a mirror can help when you are looking at hard-to-see areas.
What should I look for?
Tell your nurse, carer or doctor if you notice:
- your skin feels sore
- red patches on light skinned people
- purplish or bluish patches on dark skinned people
- swelling, especially over bony parts
- blisters
- shiny areas
- dry patches or hard areas
- cracks, calluses, wrinkles, or broken skin.
Eating and drinking
What you eat can also affect your condition. Try to eat a good balanced diet. If you are not eating properly for whatever reason, your skin can become fragile. You should eat foods from each of the following groups:
- meat, fish, poultry, or alternatives
- fruit and vegetables
- bread, potatoes, and cereals
- milk and dairy foods.
Drink plenty of fluids. Fluids stop the skin from becoming dehydrated and therefore less prone to damage.
What else can you do to help yourself?
Cooperate with any moving, turning and positioning programmes planned by the health care staff. If provided with specialist equipment, please use it as directed.
About this leaflet
Author: Sharon Thomas, Tissue Viability Nurse
Updated: July 2023
Approved: December 2023
Review date: December 2026
Edition: v2
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a
list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
