Persistent Postural Perceptive Dizziness (PPPD or 3PD)
What is PPPD?
PPPD is a cause of chronic long-lasting dizziness. It is triggered usually after a brief episode of dizziness or vertigo. Following the initial episode, the person continues to have feelings of movement, dizziness, unsteadiness, or light-headedness lasting for hours or days at a time. These symptoms are present nearly all the time, but they can be better or worse at times.
Things like sitting or standing upright and seeing busy patterns or movement often make the symptoms worse. Consequently, people with PPPD often become anxious about losing their balance or falling. They may avoid situations that make their symptoms worse, to the point where it can start to interfere with their lives.
What are the symptoms?
- Non-spinning vertigo (feeling as if you are swaying or rocking, even though you are sitting or standing still)
- Unsteadiness (feeling as if you are about to fall)
- Light-headedness (feeling woozy or as if you are going to pass out)
- Mild dissociation (feeling “spaced out” or as if you are floating).
These symptoms happen on most days for at least three months. They may last for hours at a time. They may not happen every day.
People with PPPD often feel worse when:
- They are standing or sitting upright
- They see movement, such as when they are scrolling on a phone, watching TV, looking at traffic or seeing many people walking around
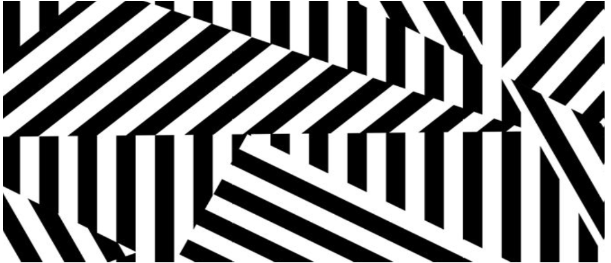
- They see complex patterns, such as a busy carpet, wallpaper, or a supermarket aisle
- They are walking or riding in a car.
Symptoms might be made worse by tiredness or paying more attention to them. They are usually persistent (they continue for a long time). The pattern of symptoms may be slightly different depending on what originally caused the PPPD.
If it was caused by an acute problem (one that lasts for a short time and then goes away) or an episodic problem (one that goes away and comes back from time to time), PPPD symptoms may start as the initial problem gets better. They may come and go at first and then become persistent.
If it was caused by a chronic problem (one that does not go away), PPPD symptoms may develop slowly and gradually get worse. People with PPPD may develop other related problems, including:
- Neck stiffness
- Problems with how they walk (their gait) fatigue (tiredness)
- Fear of falling
- Anxiety or avoidance about things that trigger dizziness for them, such as crowded places or even going outside.
How is PPPD usually treated?
Vestibular system is a sensory system in your inner ear that helps maintain balance and spatial orientation. Vestibular rehabilitation is an exercise-based program improving brain’s ability to understand the information given to it by the balance system. A combination of exercises provided by physiotherapists will be helpful.
Resuming regular activities will help your balance system recover gradually. During your daily activities avoid keeping your head in a fixed position. Instead, move as naturally as possible to allow your balance system to return to normal.
An example of some simple balance exercises you can try at home:
- Practice standing with your feet closer together, aiming to hold this position for 30 seconds. If you don’t feel steady, hold onto something for support. Once you feel balanced enough to do this without holding on, try practicing this stance while washing your hands or brushing your teeth. Can begin with holding onto support and gradually withdraw as you progress. This improves balance.
- Aim to walk outdoors each day for at least 10-15 minutes. Gradually increase the duration and include slopes or hills as you build stability. This increases connectivity between the vestibular and balance system. It is r ecommended you practice this is a quiet area and then to progress to busier areas.
- When reaching into a cupboard, make sure to look at where you’re reaching. This encourages a more natural head movement.
Start by looking at the pattern for a few minutes to get your brain used to busy visual information. Always stop when your symptoms increase. Allow the symptoms to subside before proceeding with anything else. It helps to use breathing techniques to relax. Keep in mind that If you start doing too much, too soon, it can make the symptoms of PPPD worse.
Over time you should start to find it easier to look at the pattern. If you’re finding it too easy, try making it a little bit harder by:
- Increasing the size of the busy background
- Standing up if you were sitting
- Gradually bringing your feet closer together
- Gently moving your head side to side or up and down while looking at the pattern.
Making the exercises harder will better prepare you for difficult visual environments when you are out and about. It is also important to your recovery that you gradually begin returning to busy environments, such as supermarkets. We recommend going at your own pace and building up to a full weekly shop. For example, it might be a good idea to start by only buying a few items and using a trolley for stability. Over time you will be able to shop for longer and rely on the trolley less.
The exercises should be completed in a busy visual pattern in the background such as this:
Meditation and mindfulness
Anxiety often plays a large role in 3PD. Meditation and mindfulness can help break the vicious cycle of anxiety and significantly reduce symptoms.
Mindfulness describes an awareness of ourselves and the world around us. Paying more attention to the present moment can improve your mental wellbeing and reduce the negative impact that your dizziness has on your life. Mindfulness involves sitting quietly and paying attention to your thoughts and your body, the sounds around you and the sensation of breathing.
One of the aims of mindfulness is to help you to lead a life where you no longer feel that your dizziness is ‘in control of you’. Instead of putting your life on hold until you get rid of your dizziness, mindfulness will help you live a life that is meaningful to you.
Cognitive-behavioural therapy (CBT) is a type of psychotherapy focused on the relationship between your thoughts (cognition) and behaviour. Cognition includes your conscious thoughts (which are under your control), your automatic thoughts (which may not be under your control) and your core beliefs (known as schemas). CBT teaches you how to notice and identify your thoughts and beliefs, consider your thoughts and beliefs from different viewpoints and change your behaviour patterns.
You can self-refer for CBT through the steps2wellbeing website at steps2wellbeing.co.uk
Medications
Your GP may prescribe medications like:
- SSRIs (selective serotonin reuptake inhibitors (SSRIs) such as Sertraline (Zoloft®), Fluvoxamine (Luvox®), Paroxetine (Paxil®).
- SNRIs (serotonin norepinephrine reuptake inhibitors) usually tried if two SSRIs have not worked). They are used to treat depression and anxiety.
Doctors usually prescribe these medications at a low dose and then increase gradually. If the side effects are not tolerated, speak to your doctor to consider another medication.
Contact numbers
We hope that you have found this information useful. If you have any questions or are worried about anything, please speak to the following Dorset County Hospital staff:
Dorset County Hospital Switchboard – 01305 251150
Mr Bruno Kenway 01305 255138
ENT Department: 01305 255832
Useful websites
If you search ‘PPPD or 3PD’ on your internet search engine there are many websites that explain the condition and treatment.
Vestibular Disorders Association (2024): https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/persistent-postural-perceptual-dizziness/
About this leaflet
Authors: Konstantina Karra, Specialty Doctor, Alistair Downtown, Nurse Practitioner, Stephanie Enesomi Alimasunya, FY2, Subash Palanisamy, Clinical Lead Vestibular Physiotherapist
Written: April 2025
Approved: July 2025
Review date: July 2028
Edition: v1
