Permanent Pacemaker Insertion
Why do I need a permanent pacemaker?
The heart is essentially a pump made of muscle, which is controlled by electrical signals. These electrical signals can become disrupted for several reasons, which can lead to a number of potentially dangerous heart conditions, such as:
- An abnormally slow heartbeat (bradycardia)
- An abnormally fast heartbeat (tachycardia)
- Heart block (where your heart beats irregularly because the signal that controls your heartbeat is not transmitted properly)
- Cardiac arrest (when a problem with the heart’s electrical signals causes the heart to stop beating altogether)
Heart failure (a problem with the heart’s pump function, where the doctor may recommend a pacemaker to resynchronise the heart function and help it to pump more efficiently, this type of pacemaker is known as ‘Bi-Ventricular pacemaker’ or ‘Cardiac Resynchronisation Therapy’). A Bi-Ventricular pacemaker means that both bottom chambers (ventricles) of the heart are paced at the same time.
What is a permanent pacemaker?
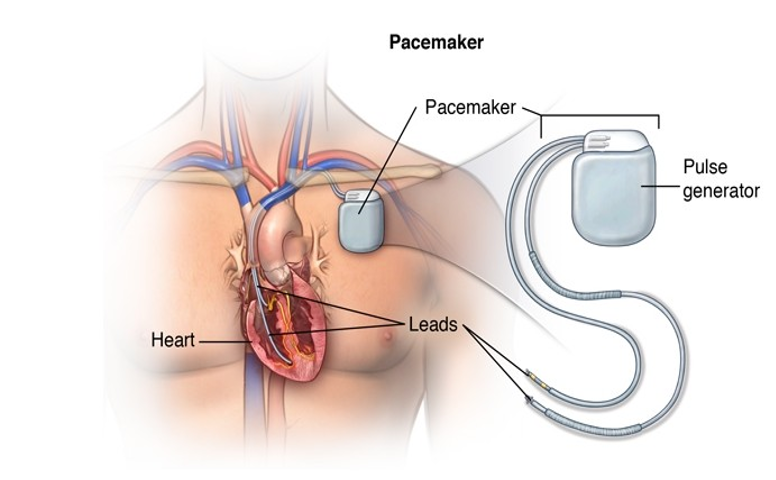
A pacemaker is a small, metal device that is about the size of a match box, or smaller, and weighs between 20 – 50g.
It consists of a pulse generator, which has a battery and a tiny computer circuit, and one, two or three wires known as pacing leads that connect it to your heart.
The generator emits electrical impulses through the wires to your heart when it detects that your heart has missed a beat or is beating too slowly. This impulse then causes your heart muscle to contract and pump. If the pacemaker senses that your heart is beating normally, it does not send out any signals and it simply monitors it.

What is Conduction System Pacing (CSP)?
This may be recommended to you as a treatment option for you by your cardiologist. The HIS Bundle and the Left Bundle Branch are very specific points along the normal electrical circuit of the heart. Positioning a wire on either of these locations, means that when the pacemaker sends out a gentle electrical impulse it stimulates the lower chambers of the heart (ventricles) in a more efficient way using the heart’s normal electrical pathways. (It could lower the chances of the heart pump becoming weaker (known as heart failure), which can affect about 9% of people after getting a regular pacemaker.)
What is Cardiac Resynchronisation Therapy (CRT)?
When damage to the heart muscle causes the heart to work inefficiently, this often leads to other symptoms, such as shortness of breath, retaining fluid in the body and reduced activities. The electrical signals within the heart can also become affected. This condition is known as heart failure.
The CRT pacemaker (also known as Bi-Ventricular pacemaker) is not like the traditional pacemakers that are used to prevent slow heartbeats. The pacemaker is implanted with the aim of totally taking over the job of the heart’s electrical conduction system and getting the lower chambers (ventricles) to pump together (resynchronised).
This type of pacemaker is not a cure for the underlying heart condition. However, research has shown that this special type of pacemaker improves symptoms for people whose heart muscle does not pump effectively.
The CRT pacemaker consists of the same metal box (pictured above) and may have up to three wires that are inserted in the heart via a vein. There is often one wire in the right upper chamber (atrium) and one wire in the right lower chamber (ventricle). In addition to these two standard wires there is a third wire placed around the back of the left lower chamber. These lead positions allow the pacemaker to coordinate the pumping of the heart.
What to expect
You will be asked to attend a pre-assessment clinic prior to your procedure. At this appointment, the nurse will take a medical history, check your blood pressure and take blood and swab tests. This helps medical staff to identify any potential problems in advance of your admission to hospital and take steps to sort them out beforehand. You will also be given more details about the procedure, including preparation and aftercare.
On the day of the procedure, you will be admitted to our day ward within the Cardiology Department, where the nurse caring for you will undertake some pre-procedure checks, including blood pressure, an electrocardiogram (ECG) to check your heart rhythm and the insertion of a small tube (cannula) into your arm. The tube is used to give you a one-off dose of antibiotics prior to the start of the procedure which helps to reduce the risk of infection. The cannula can also be used during the procedure to give any other medication.
The pacemaker is implanted in a room called a catheter lab, which looks like an operating theatre.
How is it performed?
You will be taken into the catheter lab and asked to lie flat on a table. A member of the team will attach you to a heart monitor (ECG) and place a blood pressure cuff on your arm. All members of the team will need to wear a hat and mask, but they will introduce themselves to you.
A pacemaker is usually fitted on the left side of your chest as this allows the wires to be inserted more easily. However, this can be discussed at the pre-assessment clinic if you have concerns.
Your chest will be cleaned with antiseptic solution and a sterile sheet placed over you. This will cover your face, but the nurses will be able to adjust it if needed. The doctor will inject a local anaesthetic into the skin near your collarbone. This will sting to begin with. When the skin is numb, a small cut is made just beneath your collarbone. The doctor will make a pocket by separating the skin away from the chest muscle. You may feel a tugging sensation when this is being done.
The lead, or leads, is then passed through one of the blood vessels under the skin near your collarbone. X-rays are then used to help position the lead, or leads, into the correct position within your heart. The leads are then connected to the pacemaker box, and the box is then placed into the pocket that the doctor created beneath the collarbone.
The skin is then closed with removable or dissolvable sutures. If removable sutures have been used, these will be removed seven to 10 days following the procedure at your GP surgery. The wound is then covered with a transparent dressing which allows for close monitoring of the wound at home.
The procedure can take between one and three hours, dependant on the type of pacemaker you are having.
What are the risks?
Complications with this procedure are rare; however, because it is invasive they can happen:
- Bleeding and bruising around the pacemaker site. The nurses will observe this closely and apply pressure if required to treat bleeding
- Infection – signs of redness, swelling, heat from the wound or puckering of the skin can be signs of infection. We ask you to contact the Cardiology department if you have any concerns. Early infections can be treated with antibiotics. However, serious infections can result in the pacemaker being removed. The risk of this is two in 100
- Lead displacement – this usually occurs within the first month of insertion, which is why we ask that you limit the use of your arm. This requires the lead to be repositioned and can happen in one in 100 cases
- Pneumothorax – this is a puncture to the lining of the lung and can be caused at the time the lead or leads are inserted into the blood vessel under the collar bone. This can be detected on the chest x-ray following the procedure and can sometimes rectify itself without any treatment. Very occasionally, a small drain may need to be inserted to the side of the chest to allow the lung to re-inflate. You may need to stay in hospital longer than expected. This can happen in one in 100 cases
- Arrhythmia – the heart rhythm can be disrupted during the procedure in one in 1,000 cases. This often resolves without requiring any intervention
- Cardiac tamponade – this is a collection of blood around the heart and can be treated by inserting a drain into your chest. This can happen in one in 2,000 cases
- Radiation – exposure to radiation is necessary in placement of the pacemaker wires. The risk of high doses of radiation is low, but slightly higher in Biventricular pacing and CSP as they are generally longer procedures.
If you require a bi-ventricular pacemaker or CSP (HIS bundle or Left bundle branch), then there is also the additional risk of:
- Reaction to the dye – this is rare. You will be encouraged to drink plenty of fluid following the procedure to help ‘flush’ the dye out of your system.
Will I need to stay in hospital?
Following the procedure, you will return to the day ward area. The nurses will then perform an ECG and check on your blood pressure. The wound will also be checked regularly for any signs of bleeding. You may be asked to remain in bed until a chest x-ray has been performed and checked by the doctor.
We aim to discharge you home the same day, providing that you have someone to stay with you overnight, the procedure is uncomplicated and all electrical checks on the pacemaker are satisfactory post procedure. This could be after two to three hours.
If you do not have anyone to stay with you overnight, you will be required to stay in hospital and be discharged from hospital the following morning. You will stay on the Cardiac Care Ward (CCW), and a bed will be confirmed on your admission to hospital. Very rarely, we must postpone a patient’s procedure if no bed is available to stay overnight; however, we will do our best to avoid this.
You will have your pacemaker checked before you are discharged from hospital, and you will be given a pacemaker ID card to carry with you. This contains important information about your pacemaker.
What happens after the pacemaker has been fitted?
As well as an ECG, blood pressure and close monitoring of the wound, you will have a chest x-ray within four hours of the procedure being completed. This is to check the position of the leads and to help rule out any problems.
As the wound can feel quite bruised and sore, especially for the first day or two, it is recommended that you take regular painkillers, such as Paracetamol. It is important that you tell your nurse immediately if you have any pain or discomfort.
It is important that the wound is kept clean and dry until it is completely healed. We recommend that the dressing remains in place for the first seven days.
If you notice any redness, soreness or swelling of the wound site, this should be reported straight away to the Cardiology Department as these may be a sign of infection.
Extra tissue will grow around the lead(s) in your heart after a few weeks, which will prevent the wire(s) moving out of place. As a general guide, you should not raise the arm on the same side as the pacemaker above shoulder height for the first month, or use it to lift, push or pull. Your pacemaker will be checked after one month and, if all the checks are satisfactory, you can resume normal activity with your arm.
Please discuss with the pre-assessment nurse or your cardiologist if you play sports and they will advise when you can go back to this.
It is normal for you to feel the pacemaker box underneath the skin. Try not to move the box or touch the site excessively. If you experience discomfort that does not settle, please inform the Cardiology Department and we will arrange an appointment to review this.
Can I still drive after I have my pacemaker implanted?
The Driving and Vehicle Licensing Agency (DVLA) have guidelines in relation to patients who require a pacemaker and whether they are safe to drive.
There will be some restrictions, but these will vary depending on why you have had your pacemaker fitted. It is very important that you discuss this with your cardiologist, pre-assessment nurse or cardiac physiologist, who will be able answer in more detail.
You must inform the DVLA that you have had a pacemaker implanted and it is also recommended that you inform your car insurance company.
Is there any equipment that can affect my pacemaker?
Medical treatment
Please tell your doctor or dentist, or any other person carrying out any other treatment, that you have a pacemaker. Please take your ID card with you when you go into hospital. You can also contact the Cardiology Department for advice before you go into hospital for any investigations or treatment that is not related to your pacemaker, if required. It is safe for you to have x-rays, CT scans and mammograms. Most pacemakers are now MRI safe, which means they have been demonstrated to pose no known hazards in a specified MRI environment with specified conditions of use. However, you must let the MRI team know that you have a pacemaker. If you have any concerns you can speak to the Cardiology department.
Travel
Please inform travel companies and airline staff, if you are flying, that you have a pacemaker. You may set off the alarms when passing through security gates and may be asked to show your pacemaker ID card.
Arc welding
This should be avoided. Please speak to the Cardiology Department if you have any concerns.
Magnets
Do not carry magnets or place a magnet over your chest. These can cause interference with your pacemaker.
Electromagnetic interference will not damage your pacemaker but may temporarily interfere with its settings whilst you are in contact with it. Most mechanical and electrical devices that you use in your normal daily activities will not affect your pacemaker.
Mobile phones
Some studies have shown that some mobile phones can affect the pacemaker if held within six inches of the device. It is, therefore, recommended that you do not keep a mobile phone in a coat or shirt pocket over the pacemaker. Keep the handset more than six inches away from the pacemaker. Ideally hold the phone over the ear on the opposite side to the device.
Household equipment
Most household equipment, such as, fridges, microwave ovens, radios, televisions etc will not cause any problems with your pacemaker. Induction hobs do generate electromagnetic fields, so keep a distance of at least 60cm (2ft) between the stovetop and your pacemaker. Most people should be able to use a hob if they follow these precautions, but if you are choosing a new cooker, it may be easier to pick one that does not have an induction hob.
Pacemaker clinic visits
Your pacemaker should be checked regularly, and it is important that you attend the scheduled appointments. Your first appointment will be one month after the implant and you will then be seen at least once per year, but maybe more if necessary. During your appointment, the physiologist will examine your pacemaker using a special computer programmer. This programmer will allow them to adjust the settings and monitor the battery life of the pacemaker. You will also have the opportunity to discuss any concerns you may have.
You may have the option to have a download box that you can plug in at home. This allows us to monitor your pacemaker without the need to attend hospital. You can find out more about this by asking the cardiology team.
Research
As a department we are very active in ongoing research.
If there are any clinical trials that we are taking part in and think that you may be suitable then this will be discussed with you by a member of the research team. This may also be mentioned to you in your appointment with the consultant or nurse before you attend for the pacemaker procedure.
Further information
You will be invited to a pre-assessment appointment where the nurses will be able to answer any further questions. If there is anything urgent, you can contact the Cardiology Department on 01305 255887.
About this leaflet
Author: Laura Starr, Matron, Cardiology Department
Written: March 2019
Updated and approved: February 2025
Review date: February 2028
Edition: v3
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet