Hartmann’s Procedure
What is a Hartmann’s procedure?
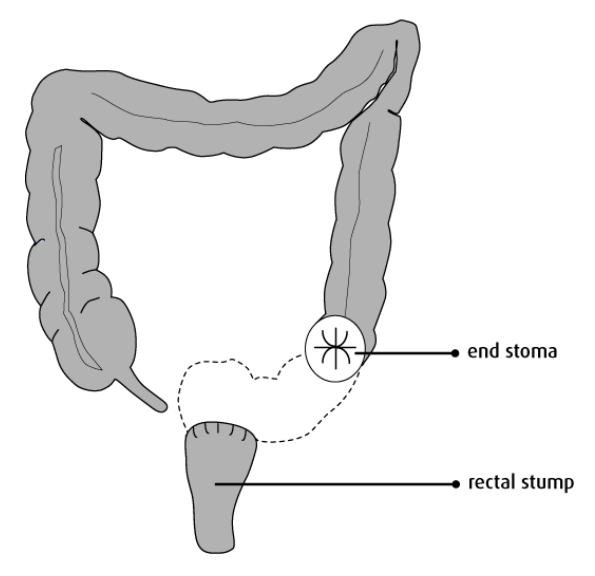
A Hartmann’s procedure is an operation to remove part of the large bowel. A cut will be made in your abdomen and your surgeon will remove the diseased area of bowel and a length of healthy bowel either side of it. An opening will be made on the left side of your abdomen and the healthy end of your bowel brought out to form a new outlet for bowel contents; this is called a colostomy, which is a type of stoma. Stools that come out of the colostomy are collected in a bag that covers it. The non-functioning end of your bowel (your rectum) will be sealed off inside your body and is often described as a ‘rectal stump’. You will see the stoma nurses prior to your surgery to discuss the stoma in more detail and answer any questions you may have.
This operation may be offered as laparoscopic (keyhole) surgery. However, laparoscopic surgery is not possible in all cases, and in an emergency, you are likely to have an open operation (traditional straight-line incision method). Your surgeon will discuss with you the type of operation that is best for you.
Preparing for your operation
Before your operation, it is beneficial for you to get yourself as fit as possible. Take gentle exercise, such as walking, and eat a well-balanced diet. If you smoke, we strongly advise you to stop as soon as you can before your surgery; you can see your GP or pharmacist for advice and products to help with this.
You can eat and drink normally up until the evening two days before your operation. The day before your surgery you should have light, low fibre foods only and avoid heavy meals and alcohol. You will also be required to drink six high carbohydrate drinks which you will be given when you come in for your pre-assessment appointment along with a more detailed information sheet on diet and bowel preparation.
You will be given a strong laxative to take the day before your operation to clear out your bowel. This will make you want to go to the toilet often, and urgently. You will be admitted to the hospital the day of your operation unless your consultant advises otherwise and will be in hospital approximately three to five days.
What risks are there in having this procedure?
Removing part of the bowel is a major operation. As with any surgery there are risks with the operation which include:
Ileus (paralysis of the bowel)
Sometimes the bowel is slow to start working after surgery which causes vomiting and delays you from eating and drinking normally in hospital. If this happens, the bowel may need to be rested and a drip (a tube into a vein in your arm) is used to replace fluids, instead of drinking. In addition, you may need a nasogastric tube (tube in your nose which passes into your stomach) so that fluid in your stomach can be drawn off. This helps to prevent nausea and vomiting and remains in place until the bowel recovers.
Possible stoma problems
The stoma could become necrotic (dead tissue) which is a result of a reduced blood supply, and some stomas can prolapse (the stoma comes out too far past the skin). In serious cases further surgery may be needed to fix these problems. There is also a chance you may develop a parastomal hernia (when the bowel pushes through a weak point in the abdominal muscle wall). Small hernias can be treated with a support garment or belt, but surgery may be needed for larger hernias.
Chest infection
After your operation it is important that you do deep breathing exercises to reduce the risk of developing a chest infection. These are some exercises to follow whilst sitting in an upright position in a chair or in bed:
- Relaxed breathing
Rest your hand on your tummy and feel it gently rise and fall with your breathing. Breathe at a comfortable pace for about 30 seconds. - Deep breathing
Take a long deep breath in through your nose.
Hold for two-three seconds. Relax, and breathe out and repeat 3 times. - Huffing and coughing
Support your tummy with your hands or a rolled-up towel. To huff, you exhale air as if you are steaming up a mirror. If you feel there is phlegm there, cough to clear it.
Wound infection
Operations of this nature carry a risk of infection and therefore antibiotics are given to you routinely during your operation.
Thrombosis (blood clot in the leg) and pulmonary embolism (blood clot in the lungs)
Being less mobile, unwell, or having surgery will put you at risk of blood clots. Your risk also increases if you are overweight, over 60 years old or have cancer.
To help reduce your risk, you will be fitted with some anti-embolic (compression) stockings for the duration of your stay in hospital. These are tight-fitting and make your blood move more quickly through your legs. You may also be given a small injection called enoxaparin (Clexane®) to help thin the blood. It is likely you will need to continue with these for a while after you return home so the nursing staff will teach you how to administer these yourself. You can help reduce your risk of blood clots by moving around as much as you are able and getting out of bed as soon as possible after your surgery. You should also avoid crossing your legs.
Bleeding
A blood transfusion may be needed during or after surgery. Very rarely, further surgery may be required.
Sickness
Some people experience nausea and vomiting after an anaesthetic and anti-sickness medications can be given to help with this.
What if you do nothing?
Your bowel condition is likely to have been causing you severe symptoms. If you choose to do nothing, you are likely to have more of the same trouble. Sometimes the disease or blockage is due to cancer and, if the operation is not performed, there is a risk that the cancer may spread to other parts of your body or cause a blockage. A blockage in the bowel can cause severe pain and perforation which is a potentially fatal situation. If you feel you could not cope with an operation for whatever reason you should discuss it with your consultant.
After your operation
You will wake up with a number of tubes attached to your body which will be removed over the next few days. These will include an intravenous infusion (drip), usually in your arm to feed you with fluids, and administer other medications such as pain relief and a catheter in your bladder to drain urine.
Anaesthetic and pain relief
Your anaesthetist will come and see you before your operation to discuss the type of anaesthetic that you will be given and what pain relief you will be given afterwards. Most major bowel operations are performed under general anaesthetic. Once you are awake, you may be given painkillers through a drip in your arm in the form of a PCA (patient-controlled analgesia) hand-held pump, or through a tube in your back (epidural).
What is the Enhanced Recovery Programme?
Enhanced Recovery is a modern, evidenced-based approach that helps you get back to full health as quickly as possible after your operation. Research has shown that the sooner a person gets out of bed and starts walking, eating, and drinking after having a major operation, the shorter the recovery time will be.
Mobilising and exercising
By being out of bed in a more upright position and walking regularly, lung function is improved and there is less chance of a chest infection after surgery. It also improves circulation, reducing the risk of blood clots and helping bowel function return to normal. Once you are back from theatre and awake, you will be encouraged to sit out in a chair as soon as possible. The ward staff will help you with this.
When you are sitting in the chair or lying in bed you should do frequent leg exercises, pointing your feet up and down and moving your ankles as if making circles. It is important to take regular walks during the day once you feel ready. The ward staff can help and, if required, the physiotherapist will check that you can manage a flight of stairs prior to your discharge. Try and wear your own day clothes after your operation as this can help you feel more comfortable and positive about your recovery.
It is important that your pain is controlled so that you can walk about, breathe deeply, eat and drink, feel relaxed and sleep well. Please let the ward staff know if your pain is not manageable so that they can help you.
Chewing gum
Chewing gum after bowel surgery is encouraged as recent studies have shown that this can assist the bowel to return to its normal function. Chewing gum can also help disperse trapped wind and the colic type pains that can sometimes occur after a bowel operation. You are advised to chew gum for 10-15 minutes, three times a day, until your bowel function returns to normal. Please be aware that sugar-free gum can cause significant wind and bloating in some people; if this is the case try a full sugar variety of gum.
Eating and drinking
After your operation, you need extra nourishment to help your wounds heal, reduce the risk of infection and help you recover. High calorie/high protein drinks will be given to you after your operation to supplement your diet (these are not a substitute for solid food).
You will be encouraged to start eating as soon as you feel able after surgery. You may find that you do not have much of an appetite at first. If you feel sick, let the ward staff know so that anti-sickness medications can be prescribed. There is no hard and fast rule about what you should or should not eat. Little and often is usually better than large heavy meals. Food with a low residue (low fibre) and easily digested is usually best at first. You may find that spicy food and a lot of salad or fruit will upset you. The stoma nurses will give you further dietary guidance when they visit you on the ward.
Going home and getting back to ‘normal’
Having an operation can be a stressful experience, physically and emotionally. In the first weeks it is normal to have some days where you feel low in mood. Some people find it takes a few months to adjust emotionally to the surgery, but things will get better. You are likely to feel tired and weak for a while, but there is no need to stay in hospital. However, it may be necessary to make sure that there is someone available to help with getting meals, cleaning your home and shopping. If you have any concerns about this, please contact your colorectal nurse for advice prior to your operation. Everybody recovers at a different rate, and it may be many months before you feel back to your normal self.
If you experience difficulties with passing urine or sexual activity, discuss this with your GP or colorectal nurse as help is often available.
Driving
You are advised not to drive for four to six weeks, and then only if you are able to apply the brake in an emergency without discomfort. We recommend you check with your insurance provider in case they have specific policies following a ‘major operation’.
Contact numbers
We hope that you have found this information useful. If you have any questions or are worried about anything, please speak to the colorectal cancer nurse specialists on 01305 253144 or email colorectalcancernurses@dchft.nhs.uk
You can also contact the stoma care team on 01305 255152, Monday to Friday, 8.30am to 4.30pm.
Useful links
Bowel Cancer UK
bowelcanceruk.org.uk
Macmillan Cancer Support
macmillan.org.uk
About this leaflet
Author: Eloise Coward-Lane, Associate Colorectal Nurse Specialist
Written: May 2023
Approved: September 2023
Review date: September 2026
Edition: v1
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientexperience.leaflets@dchft.nhs.uk
Print leaflet