Cardiac Re-Synchronisation Therapy with Defibrillator (CRT-D)
This leaflet has been written for those who are about to have a specialised pacemaker device called ‘cardiac re-synchronisation therapy with defibrillator’ (CRT-D) procedure. We will use the abbreviation CRT-D to refer to it throughout this leaflet. It is the aim of this leaflet to help you and your family/close friends understand what a CRT-D is and how it works. It will explain what can be expected during the procedure and consider the benefits/risks of having the device. The leaflet will also discuss the longer-term issues about living with a CRT-D device. You will have an opportunity to discuss all these issues further with your nurse and doctor before going ahead with the procedure.
What is CRT-D?
A CRT-D device is about 5cm x 5cm and weighs about 75 grams. It is a sealed unit containing a battery-powered electronic circuit. The CRT-D is connected to the inside of the heart by two or three leads. The leads are very fine, flexible wires, which are covered in a layer of plastic or silicone.
The leads are connected to the heart by a small hook or screw that is attached to the heart muscle. The leads heal into place, becoming permanent and stable, within four weeks of having it fitted.
Why do I need a CRT-D?
Doctors recommend having a CRT-D if your heart does not pump as strongly as usual (heart failure) and you have experienced, or are at risk of experiencing, an abnormal, fast heart rhythm that can cause you to become unwell, unconscious or for your heart to stop beating. These rhythms are called ventricular tachycardia/fibrillation and will be described later on in this leaflet. Firstly, we need to think about how the heart works normally.
How does the heart work normally?
The heart pumps blood (that contains oxygen) around your body. The heart has four chambers, two at the top (right and left atrium) and two at the bottom (right and left ventricles).
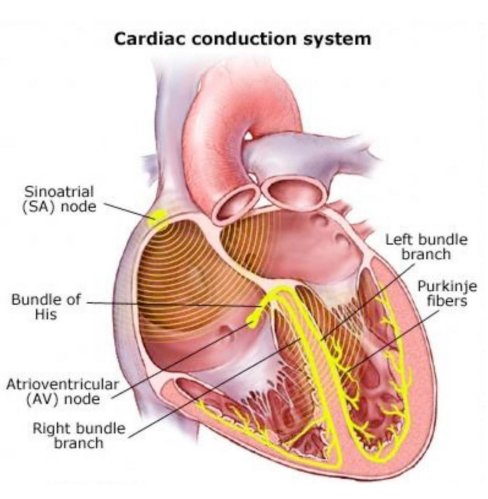
Your heart needs an electrical impulse to generate a heartbeat (make it pump). The electrical impulse starts in the right atrium (see below) in a bundle of tissue called the sinoatrial node. The impulse then travels across the top chambers and down to the bottom chambers causing these chambers to pump blood around the body.
The heart normally beats regularly and slowly at rest but faster during physical and emotional activity. In some people, the bottom chambers of the heart can suddenly change rhythm and beat very quickly; the general term for this is arrhythmia. This can mean that the heart is unable to pump enough blood around the body. The defibrillator element of the CRT-D can treat two types of rhythm disturbances; ventricular tachycardia and ventricular fibrillation.
What is ventricular tachycardia (VT)?
Ventricular tachycardia (VT) is an abnormal, fast, regular rhythm that is caused by abnormal electrical impulses from the bottom chambers of the heart. During VT the heart beats a lot faster than normal, which can reduce the pumping action of the heart and lead to poor blood circulation. This may cause symptoms of faintness, dizziness, shortness of breath or chest pain. If the rhythm persists it may cause unconsciousness.
What is ventricular fibrillation (VF)?
Ventricular fibrillation (VF) is different from VT because it is often faster and it is chaotic.
The bottom chambers, in VF, get so many impulses that the heart ‘quivers’ instead of squeezing so it cannot pump any blood around the body. Consciousness will be lost within seconds and this rhythm is fatal unless an electric shock (defibrillation) is delivered to restore normal heart rhythm. People without an ICD would need to wait for the ambulance to arrive to receive defibrillation. People with an ICD can receive treatment within seconds of there being a problem. Most people who have an ICD live a normal life with very few restrictions. The aim of implanting the ICD will be to give you a built-in ‘life-saver’ that can deal with life-threatening heart rhythm problems.
What is heart failure?
Heart failure is a medical term used to describe a condition where the pumping action of the heart is weak. This can cause breathlessness, ankle or leg swelling, increased tiredness and difficulty sleeping at night due to breathing problems. Some people with heart failure can develop a condition called dysynchrony. This means that the ventricles (bottom chambers of the heart) do not squeeze in time with each other, which can worsen heart failure symptoms. ‘Cardiac re-synchronisation therapy’ (CRT) treats dysynchrony and may improve your symptoms.
Why do I need a CRT-D?
Even though you are taking regular medication, you may still be getting heart failure symptoms. A CRT-D is designed to work with your medications to improve your symptoms by helping your heart to squeeze in a more coordinated way. It is hoped that you will feel better and have an improved quality of life. The CRT-D also provides protection against sudden cardiac death caused by abnormal heart rhythms from the bottom chambers of the heart. The aim of implanting the CRT-D will be to, hopefully, improve your symptoms and you will also have a built-in ‘Life-Saver’ that can treat potentially life-threatening heart rhythm problems.
How does a CRT-D work?
- The cardiac re-synchronisation (CRT) element of the device aims to improve heart failure symptoms by providing tiny electrical impulses (pacing) to both lower chambers of the heart. This improves the pumping/squeezing action of your heart and ensures your heart rate does not go too slowly.
- Stores a record of fast heart rhythm problems and any treatment you receive from the device.
- Anti-tachycardia Pacing (ATP). If the heart rate goes too fast in the bottom chambers, the ICD can pace faster than the abnormal rhythm, which can sometimes stop the VT without you even noticing.
- Defibrillation shock. If the rhythm is VF, or the VT is too fast, the CRT-D will deliver an electrical shock (defibrillation) to the heart muscle through the lead that sits in your right ventricle. This should end the serious or life-threatening heart rhythm and restore normal heart rhythm. People have different ways of describing a CRT-D ‘shock’. It has been described as feeling like a firm thump or a kick in the chest or back. A shock may be painful or distressing, although the pain only lasts a few seconds. It is natural to feel anxious, but try to stay calm. Remember that it is the abnormal heart rhythm that is dangerous rather than the CRT-D. You cannot harm anyone else if you have a shock whilst you are touching them; they may feel a tingle and feel you move, but they will not receive an electric shock. You will find advice later on in this leaflet about what to do if
you have needed a shock from your CRT-D. - Cardiac re-synchronisation therapy. Small electrical impulses (pacing) is delivered to both lower chambers (ventricles) to stimulate them to contract in a coordinated pattern. This causes the heart to pump blood to the rest of the body more efficiently.
Inappropriate CRT-D (defibrillation) shocks
It is rare, but the CRT-D sometimes incorrectly analyses your heart rhythm as needing a shock when it does not need one; this is referred to as an “inappropriate shock”. It will feel the same as a normal shock, but your treatment (medication and/or CRT-D settings) will need to be reviewed to try and avoid you receiving further inappropriate shocks. We would let you know if we thought a shock had been inappropriate.
Are there any risks with having a CRT-D fitted?
As with any procedure there are risks involved and, although all measures are taken to minimise the chances of complications, it is important to be aware that occasionally complications can occur with this procedure:
- Bleeding or bruising is very common
- It is possible that the leads will become dislodged; the chance of this happening can be reduced by not lifting your arm above your head, behind your back or lifting heavy objects for four weeks after the procedure
- As with any surgical procedure there is a risk of infection
- Rarely a lead can puncture the lung, which can be corrected by inserting a chest drain
- Very rarely a lead can puncture the heart wall, which could then cause fluid to build up around the heart in the fibrous sac (pericardium) that surrounds the heart. If this does occur, a temporary pericardial drain may need to be used
- Rhythm problems during the procedure sometimes occur but they can be dealt with by using the defibrillator machine if needed
- It is possible to be allergic to the dye that is used to see the main vein on the x-ray pictures. This would be treated promptly if it did occur. If your kidney function is poor, the dye can sometimes worsen its function. We will do a blood test beforehand and, if this is an issue for you, we can give you extra fluid through a drip during the procedure, which can help.
Please be reassured that all of these risks are extremely small. If you have any further concerns about these risks please discuss them with your doctor.
Consent
We must obtain your written consent to carry out this procedure before it takes place. Staff will explain all the risks, benefits and alternatives before asking you to sign a consent form. If you are unsure about any aspect of the treatment proposed, please do not hesitate to speak with a senior member of staff.
How do I prepare for the procedure?
You will see the arrhythmia nurse specialist who will:
- Check your medical history and current condition
- Help you understand the procedure
- Discuss the benefits and risks of going ahead with the procedure
- If necessary, request further tests.
X-rays are used during the procedure, so it is important to inform the team looking after you if you think there is a possibility you may be pregnant. Please remember to bring a list of all your current medication with you to all of your appointments. It is a good idea to always carry an up-to-date list of your medication with you at all times.
On the day of admission
You should have nothing to eat (including chewing gum) for six hours before your CRT-D implant procedure. You can drink ‘clear fluids’ until two hours before. Regular medication should be taken as usual; however, if you are a diabetic and/or taking warfarin/anticoagulation (apixaban, dabigatran, edoxaban, rivaroxaban), instructions on these medications will be discussed with you when you are seen by the arrhythmia nurse specialist.
You can reduce the chance of infection by having a thorough bath or shower on the morning of the procedure, but do not use any oils or body moisturiser. You will usually be asked to report to the cardiology reception (South Wing 1 entrance) on the day of your procedure. The day ward team will welcome you into the cardiology day ward and help you prepare for the procedure.
You will be asked to change into a hospital gown. Your blood pressure, pulse and heart tracing (ECG) will be recorded. The skin around your chest, where the CRT-D will be inserted, will be cleaned with an antiseptic fluid. Prior to cleaning the skin on your chest, we use clippers to remove hair around the site of the operation. We use clippers to avoid bleeding issues that can occur with shaving. A needle (cannula) will be put into a vein in your hand or arm so that medication such as antibiotics, sedation and painkillers can be given to you.
What does the procedure involve?
The procedure is done in a special x-ray room that is also an operating theatre. You will be taken into the room and greeted by the team looking after you (doctors, a cardiac physiologist, radiographer and nurses).
Sometimes there may be other people in the room observing for teaching purposes; please inform the staff if you have any objection to this. The procedure will take one to three hours to complete. Your chest will be cleaned again and sterile towels will be draped over you. The CRT-D is almost always implanted on the left side of your upper chest. The doctor will inject a local anaesthetic below your left collarbone in order to make the area feel completely numb. Initially the injections will sting a little. Sedative medication, to make you feel very sleepy and relaxed, can be given to you during the procedure if you need it.
Once the area is numb, the doctor will make a small cut and create a pocket under the skin where the CRT-D will be placed. This might cause an uncomfortable tugging/pulling sensation, but should not be painful. More local anaesthetic can be given if it is painful, so please let your doctor/nurse know if you are in pain. The doctor will then find the vein and pass the defibrillation lead down into the bottom chamber of the heart (right ventricle). The second lead will be placed in the coronary sinus vein and, although this vein lays on the outside surface of your heart, the lead enters from inside the heart. To find the coronary sinus a special dye that shows up on the x-ray image is used. Sometimes this lead can be difficult to place and is sometimes not possible. If it is not possible to place the lead, your consultant will discuss onward options with you. If three leads are being used, the final lead is then placed into the top chamber of the heart (right atrium).
The lead positions are checked by using x-ray images and by running some device checks. The leads are then secured into position with the device being placed in the pocket, under the skin or muscle made earlier. The area will then be closed with stitches (usually dissolvable and a clear dressing placed over the skin for protection. You will return to the day ward to recover. You will usually stay in this area and have a chest x-ray and CRT-D check before going home later in the day.
What happens after the CRT-D is fitted?
Once you have returned to the day ward, you will remain in bed for a couple of hours, depending on how sleepy you are. The wound may feel sore once the local anaesthetic has worn off and you will be able to have painkillers if the wound remains uncomfortable. It is important that you do not lift your arm above shoulder level on the same side that the CRT-D has been fitted for at least one month.
Please remember not to use your arm to push yourself off a chair/bed, push or pull heavy objects or carry heavy bags. This will help to reduce the chance of leads moving out of position.
You will be given a CRT-D identification card and details of further follow-up appointments. Please ask the physiologist or arrhythmia nurse specialist if you have any questions or concerns about the device. You will be able to go home once the doctor has seen you and confirmed that you are ready.
Making a good recovery
You will be encouraged to get back to your normal daily life as soon as possible after having the CRT-D inserted. After an initial period of recovery (approximately one month), you will be able to return to normal life. Some people notice an immediate improvement to their symptoms and for others it is more gradual. Occasionally people do not notice an improvement with their symptoms. Your response to the therapy will be assessed further at the follow-up appointment. If you have not noticed improvement to your symptoms, further programming of the device will be considered to try and optimise the device settings for you. The CRT-D will not prevent you from taking exercise as before and there is no reason for it to affect your sex life. Even if it delivers a shock during close contact, it will not cause harm to your partner. It is not unusual to feel anxious, elated, fearful, angry, relieved and all sorts of other emotions. Often close family members and friends are experiencing similar emotions. Talking about your concerns and feelings with someone else can often make it easier for you to adjust to living with a CRT-D.
Using your arm
For the first four weeks after the procedure do not lift the arm nearest to your CRT-D site above shoulder level or use it energetically, as not doing so will help to prevent bleeding and movement of the CRT-D leads. Activities such as hanging clothes on a washing line, pushing a vacuum cleaner, pushing yourself up from a chair/bed, carrying heavy objects or putting your arm behind your back should also be avoided for the first month. When you are dressing, put your clothes over the arm near your CRT-D site first, so you are not pushing your hand above your head or behind your back. Do gentle arm exercises to ensure that the movement of the shoulder does not become restricted.
Wound care advice
Your wound has been covered with a clear dressing and this should be left in place. If it starts to peel away, please go to your GP/practice nurse to renew it, as keeping the dressing intact can help to reduce the risk of infection. If the wound is painful, take regular painkillers as prescribed. The stitches will dissolve by themselves and the dressing can be removed seven days after the CRT-D has been inserted.
Check your wound for:
- Soreness
- Increased swelling and/or warmth
- Redness
- New oozing/bleeding from the wound
- Skin ulceration
- Raised temperature.
If you spot any wound problems, come back to the Cardiology Department immediately between the hours of 8am and 5pm, Monday to Friday, but you need to ring us beforehand to let us know that you are coming, on 01305 255288. Outside of these hours please go to the Emergency Department. Wound problems can occur even months/years after implant, so do keep checking the wound and, if in doubt, we would like to see you.
Do not have a bath until your wound has healed. You can have a shower, but do not wash the wound area with soap, flannel, bath mitt etc. Stand with your back to the flow of water; dry off any splashes of water to the wound area straight away. Do not put direct pressure on the wound, such as lying face down, whilst the wound is still sore. You can wear a seat belt on the opposite side to the wound. Having a CRT-D does not make you exempt from wearing a seatbelt. The CRT-D is of small size and weight, but you may be able to feel the device and the leads attached to the device under the skin. However, do not try to move the device or the leads.
When will I be able to drive?
On a standard driving licence you will have to stop driving for either one month or six months following insertion of the CRT-D. The length of time for which you are unable to drive depends on the reason why the CRT-D was fitted in the first place, and the Driver Vehicle Licensing Authority (DVLA) sets out specific guidelines for this. Please confirm with the arrhythmia nurse specialist if you are unsure which regulations apply to you. If your CRT-D did need to deliver a shock when you were driving it could put you and others at risk. You must inform the DVLA and your insurance company that you have had a CRT-D inserted; failure to do so will invalidate your insurance. You must also inform the DVLA if the CRT-D delivers a shock, as you will then not be able to drive for at least another six months. Although it is your responsibility to inform the DVLA, please do not hesitate to contact the arrhythmia nurse specialist if you require assistance with filling in any forms that the DVLA may send you.
Do I still need to take medication when I have a CRT-D?
After having a CRT-D fitted, some of your tablets may be changed, but in general you will still need your tablets/medicines alongside the CRT-D. Never discontinue any drugs without talking to your doctor.
Do I need to tell anyone about my CRT-D?
Before you leave the hospital you should be given an ‘Identification Card’. It is important to carry this Card at all times as it holds information about the make, model and settings of the CRT-D. Your GP will be informed by the hospital that you have a CRT-D. You will need to inform anyone treating you medically (eg doctors, dentist, ambulance or hospital staff) that you have a CRT-D. It may be important to inform your employer – see section about returning to work below.
When can I return to work?
There are no particular rules about when to return to work, as everyone is different. Speak to your doctor about returning to employment and discuss your CRT-D with the Occupational Health Department or Health and Safety Advisor where you work, if necessary.
Can I travel abroad?
Whether you are safe to travel/fly depends on your overall health; the CRT-D itself is not a barrier to travelling. At the airport always show your CRT-D Identification Card to security staff and ask to be searched by hand. Hand-held wand-type devices can temporarily interfere with your CRT-D and should be avoided if possible. You can walk straight through the metal detector archway, but must not linger underneath or touch the archway. The metal casing of the device may cause the security alarm to be activated. The body scanners that some airports use are safe to walk through. You will need valid travel insurance that includes cover for your CRT-D. Although we are unable to recommend any particular company, we can provide a list of companies that are happy to consider insuring people travelling with a CRT-D. If you are concerned about going on holiday with a CRT-D, the arrhythmia nurse specialist can provide addresses of national and international CRT-D centres that you can contact if you require assistance while you are away. Please inform the arrhythmia nurse specialist of your planned holiday in advance so that the relevant
information for your destination can be obtained.
What do I do if I hear my CRT-D alarm?
The CRT-D device has an inbuilt alarm system to notify patients of the need to seek assistance. Alarms may sound for a number of reasons, which can only be diagnosed by doing a CRT-D check. If you hear your device alarm, make contact with the Cardiology Department or arrhythmia nurse specialists immediately (see contact numbers at the end of the leaflet).
What should I do after a shock from the CRT-D?
If you receive a shock from the CRT-D device, it is doing the life-saving job it was designed to do. Some patients experience palpitations and/or feel dizzy or light-headed before they receive a shock. If this is the case, you should inform someone that you are feeling unwell and sit or lie down. If you receive a shock from your CRT-D while conscious and then feel better afterwards, the CRT-D is functioning properly. You still need to contact the CRT-D Help Line on 01305 255815 (within normal office hours) as we will need to arrange to check your device and review exactly what happened. If this occurs at night or at the weekend and you do not feel unwell, you may wait until the next working day before contacting us.
Sometimes people have a shock without feeling any other symptoms and, in this situation, it may be that the CRT-D has delivered a shock wrongly so it needs to be checked. You would need to contact the CRT-D Help Line (within normal office hours) or attend the Emergency Department (A&E) if this happens outside of office hours, as it needs to be checked as soon as possible.
If you continue to feel unwell following a shock, have blacked out, or if you are given more than one shock, dial 999 for an ambulance. It is very important to take your CRT-D Identification Card and your current medication list with you whenever you attend hospital.
If the hospital is not Dorset County Hospital, please make sure we are contacted to let us know you have had a shock. In all cases where your CRT-D has delivered a shock, you will not be able to drive until the CRT-D centre confirms that you can.
Will any equipment affect my device?
Electrical equipment and magnets have electromagnetic fields around them that are usually weak and will not affect your CRT-D. Strong electromagnetic fields can cause interference and affect the functioning of your CRT-D. Most everyday mechanical and electrical equipment will not affect the function of the CRT-D as long as they are properly maintained.
It may be necessary to discuss your working environment and precautions may need to be taken with certain pieces of equipment. Household appliances like radios, cookers (except induction hobs), computers, dishwashers and microwaves can all be used as long as they are in a good working condition. Electric hand-held drills need to be kept 12 inches away from the CRT-D and use of the hammer function avoided.
You need to avoid:
- Direct contact with car ignition systems whilst the engine is running (during car maintenance)
- Welding equipment
- High powered radio equipment and television transmitters
- Standing next to large stereo speakers (eg those found at concerts)
- Carrying strong magnets or placing a magnet over your chest/back
- Power generators
- Induction hobs.
Mobile phones are safe, but should be kept approximately 15cm (6 inches) from the CRT-D. When making phone calls, the mobile should be held to the ear on the opposite side to the device and, when carrying a mobile phone, do not store it in your shirt/jacket pocket on the same side as the CRT-D.
Anti-theft security gates at shops and banks provide a very small risk of interfering with the CRT-D. Walk through doorways normally, but do not wait around in the area of the security system/shop doorways.
Most medical and dental tests will not affect your CRT-D, but some equipment may cause interference, so remember to tell the person treating you that you have a CRT-D. The procedures where special precautions need to be taken or that you should avoid include:
- Most scans are safe, including X-Ray and CT scans. In the past MRI scans were not used on people with CRT-Ds however, most of the new models can withstand MRI scanning; check with arrhythmia nurse specialist or cardiac physiologists
- Diathermy and electrocautery are generally used in surgical procedures and may affect the function of your CRT-D. Adjustments can be made to the device before any surgical procedure is done to prevent any problems
- Special precautions will need to be made to protect your CRT-D if therapeutic radiation treatment for cancer is needed
- Transcutaneous electrical nerve stimulation (TENS) is used for pain relief and can affect the function of your CRT-D and may need to be avoided
- Avoid using electronic body fat scales.
Most other medical procedures will not affect your CRT-D. If you have concerns about the safety of equipment in relation to your CRT-D, please contact the arrhythmia nurse specialist or CRT-D Help Line.
What follow-up care do I need?
Your CRT-D will need to be checked regularly, and your first check will be about four weeks after it has been implanted. After that it will usually be checked every three to six months. Follow-up appointments provide a good opportunity for you to ask any questions and discuss concerns. Usually we can do the check through a remote monitor that you keep at home, but we will always see you in clinic at least once every year.
Among other checks, the life of the battery is monitored at every follow-up appointment and it will not be allowed to run down to nothing. The battery life of a CRT-D is approximately five to ten years. Having the battery changed is a similar procedure to having the CRT-D inserted except that in most cases new leads are not needed.
Can CRT-D shock therapies be turned off?
Sometimes the CRT-D shock therapies and anti-tachycardia pacing need to be switched off. This can be done simply and painlessly and this is often done before a surgical procedure to avoid patients having shocks when they do not need them. Shock therapies may also be turned off if we know that someone is approaching the end of their life when they feel that a life-saving shock from the device would not be helpful.
Although it can be difficult to talk about, planning ahead in these circumstances is important. Please speak with the arrhythmia nurse specialist, your GP or other members of the team if you feel you need to discuss this issue.
Further help and information
Having a CRT-D implanted gives you a lot of information to think about. The arrhythmia nurse specialist is available to discuss any further questions or concerns regarding your planned procedure. In the event of an unrelated medical problem please call your GP and of course, in an emergency, please dial 999 and ask for an ambulance.
West Dorset ICD Support Group
Every three months the West Dorset ICD support group meet. This is a group for people with an ‘Implantable Cardioverter Defibrillator’ (ICD) and their families. Your CRT-D device contains an ‘Implantable Cardioverter Defibrillator’. Meeting with others gives you another source of support and advice. Please ask the arrhythmia nurse specialist for details of location and dates.
Contact numbers
We hope that you have found this information useful. If you have any questions or are worried about anything, please contact the following Dorset County Hospital staff:
CRT-D Help Line: 01305 255815
8am – 6pm, Monday to Friday
You will be asked to leave a message – please remember to include your contact telephone number
Arrhythmia nurse specialists: 01305 254920 or arrhythmianursespeci@dchft.nhs.uk
9am – 5pm, Monday to Friday
Day Ward – Cardiology Department: 01305 244990
8am – 6pm, Monday to Friday
Cardiology Department reception: 01305 255288
8.30am – 5pm Monday to Thursday and 8.30 am – 4.30pm Fridays
Useful websites
British Heart Foundation: 08450 708070 or www.bhf.org.uk
Arrhythmia Alliance: 01789 450787 or www.arrhythmiaalliance.org.uk
About this leaflet
Author: Kay Elliott, Arrhythmia Nurse Specialist
Written: January 2021
Approved: February 2021
Review date: February 2024
Edition: v1
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet