Anti-VEGF Intravitreal Injection Treatment
This leaflet explains the procedure of having an intravitreal injection to the eye of anti-angiogenic (anti-VEGF) drugs. It will help you to understand the procedure and the care that you will receive.
If you would like additional information about the eye, and what the procedure involves, please speak to one of the doctors or nurses. They will be more than happy to help.
What is an intravitreal injection and why do I need one?
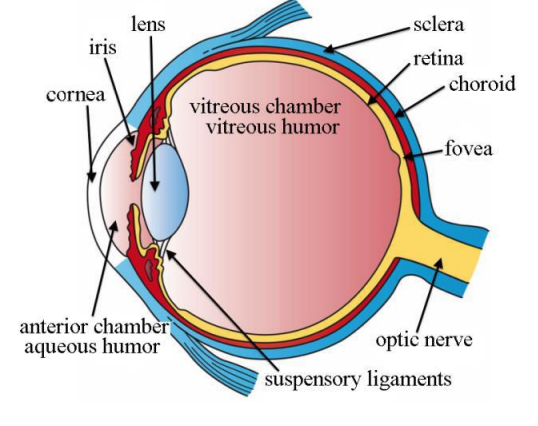
There are several conditions that may benefit from these specialist injections. An intravitreal injection involves a drug being injected through the white of the eye (sclera) into the jelly (vitreous) at the back of the eye.
Conditions such as wet age-related macular degeneration can result in growth of new abnormal blood vessels inside the eye.
These blood vessels can bleed or leak fluid underneath or into the retina. Other conditions such as diabetes mellitus, or blockages of the
retinal veins (retinal vein occlusion), can cause damage to retinal blood vessels, leakage of extra fluid and so abnormal swelling of the
central part of the retina (macula).
The above conditions can result in a build-up of blood or fluid into or under the retina. This can cause problems with the eye sight, especially if the macula is affected.
The macula is the central part of the retina and is used for our fine vision, such as reading or seeing faces. Severe or longstanding fluid and bleeding can cause permanent loss of central vision.
The injection of anti-VEGF drugs into the eye, such as ranibizumab (Lucentis) or aflibercept (Eylea) can slow or stop the growth of abnormal blood vessels and leakage. They are effective in reducing blood vessel growth or drying the macula in the majority of people.
Anti-VEGF medications may not restore sight that has already been lost and they do not always prevent further loss of sight caused by the underlying eye disease. Every patient is different and some people may only need a small number of injections while others may require ongoing treatment with repeated injections to maintain the eye sight.
Where do the injections take place?
The injections are done as an out-patient procedure in the Eye Department. You will be given the date, time and location details by letter or telephone call.
Who will give the injection?
The injection will be given by a trained health care professional or by a doctor.
How do I prepare for the procedure?
- Arrange for someone to drive you to and from your appointment
- Please bring your appointment letter and a copy of your repeat prescriptions
- Please bring your glasses
- Please bring a snack if you are diabetic
- Wear loose, comfortable clothing suitable for lying down
- Do not wear eye makeup or use false eyelashes on the day of the procedure and for three days after the injection
- Please have clean cotton wool pads and artificial tears ready to use for when you get home after the procedure
- Please notify staff prior to arrival if you have had a heart attack or stroke in the last three months
- Please notify staff of any allergies you have
- Please notify staff on the day if you have had any changes to your health, any signs of infection, or if you have been prescribed antibiotics for a current, active infection.
What will happen on the day of the procedure?
On arrival you will see the macular nurse who will go through the pre-procedure checks to ensure we can safely perform the injection that day.
You will have your vision tested, your eye pressure checked and a questionnaire will be carried out. Other tests may be performed, such as an eye scan.
Once the pre-procedure checks have been completed by the macular nurse, you will return to the main seating area where you will wait to go into the procedure room.
Inside the procedure room
Local anaesthetic eye drops are used to numb the surface of the eye, followed by antiseptic eye drops to reduce the risk of infection.
The eyelids and skin around the eye are cleaned with an antiseptic solution and a small, sticky drape is applied to cover your eye to keep the area sterile. A small clip (speculum) is then placed to keep the eye open so you cannot blink. The injection site is marked and the drug is injected.
It is important that you keep your eye in the position you have been asked and to keep still until advised otherwise.
After the injection, you will have your sight checked to make sure you can count fingers or see hand movements. Sterile water is then used to wash out the antiseptic. The lid clip and drape are removed and the skin around your eye is cleaned. Before you leave, you will be advised if your next appointment is a clinic follow up or another injection. A letter or telephone call will follow giving you details of your next appointment.
Post injection advice
Your vision will be blurry and you may be aware of the clear medication. You may also notice a few black dots. Do not be alarmed by these as they are caused by tiny air bubbles in the medication. The medication and any air bubbles will gradually disperse over the next 24-48 hours.
Your eye may be watery, a bit sore and slightly red, but this should settle over the next few days. We advise that you use artificial tear drops as often as you need to help soothe your eye. Allow 30 minutes between the artificial tear drops and any other eye drops you may need to use. You may need to use artificial tears for around three days after your injection.
You can also take simple pain relief if required.
Bathe your eye to keep it clean post injection as it may be watery or slightly sticky. Use clean cotton wool pads and cooled boiled water. Dip the cotton wool pads into the cooled boiled water and, with the eye closed, wipe from the nose outwards and repeat with another clean cotton wool pad. Do this at least twice a day for three days post injection. Do not use a flannel as this could increase your risk of infection.
You may wash your hair and bathe or shower, but close your eyes tightly to avoid getting water or shampoo in the eyes.
You can carry out your normal day to day routine and may use the eye normally for reading and watching television etc.
You may drive a car after 24 hours if your eye is comfortable and vision is clear enough to be safe by the DVLA standards.
To minimise the risk of infection getting inside your eye, exercise caution for three days following the injection:
- do not rub your eye post injection, especially for the first 60 minutes, as you will not
- have full sensation due to the anaesthetic drops and could cause harm
- do not use eye make-up or use false eyelashes for three days post injection
- do not use contact lenses for three days post injection
- do not go swimming for three days post injection
- we advise that you allow at least 48 hours before going on an airline flight post injection.
Important
If you experience any of the below symptoms:
- Severe eye pain
- Signs of infection, such as increasing eye redness, yellow/green coloured discharge
- If your vision worsens, including sudden onset of flashing lights, a shower of floaters or a curtain effect over your vision.
Please call the Eye Department immediately on 01305 255192 between the hours of 8.30am and 6pm Monday to Friday and 8.30am and 1pm Saturdays.
Out of hours, attend your nearest Emergency Department.
Contact numbers
For any questions/post injection advice and follow up clinic appointment enquires please call:
Macular Failsafe Supervisor: 01305 253166
There is an answerphone service available for this number. Please leave your details and we will respond to you as soon as possible.
For booking or amending your intravitreal injection appointments, please contact:
Admissions office: 01305 255761
About this leaflet
Author: Tony Brett, Intravitreal Injection Nurse Specialist
Written: November 2019
Approved: January 2020
Review date: January 2023
Edition: v2
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet