Advice for Patients with a Knee ROM Brace
Due to your recent knee injury, you have been fitted with a range of motion (ROM) knee brace. This brace is used to treat a variety of knee injuries from knee sprains, ligament repairs to fractures. The brace has hinges at the knee joint that can be set at various ranges of flexion (bending knee) and extension (straightening knee) throughout the course of your treatment. This allows gradual increase in movement over time to protect your knee joint and prevent instability. The brace supports and protects the knee from a ‘twisting motion’. The brace is removable, which allows for washing, physiotherapy and wound inspections.
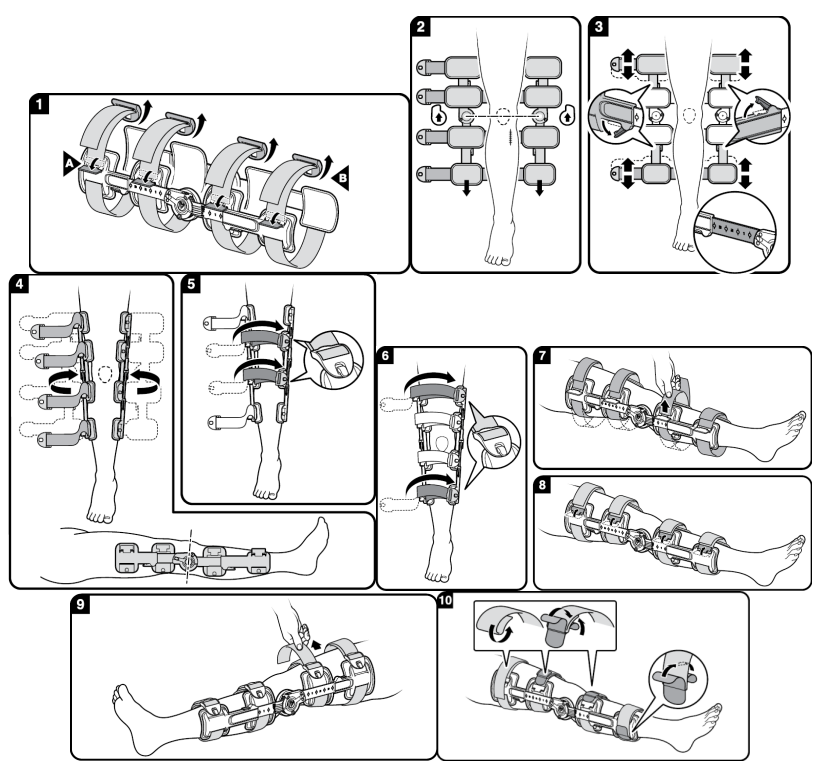
Application of your knee ROM brace
The first application of your brace should be carried out by an experienced clinician and will be explained to you. Please follow the below steps if you need to make any adjustments.
- Unlock strap clips (A), Unclip buckles (B).
- Spread hinge bars apart, lay brace out flat, position device with knee centred between hinges. Position the brace so the hinges are facing in the direction indicated and the small calf pads are towards the feet.
- Loosen friction clips on the telescoping bars. For proper fit, slide upper and lower telescoping hinge bars to accommodate leg length. Lock friction clips. Hinge bar length indicators assist in verifying the consistent length selection on thigh and calf.
- Position hinge bars laterally and medially to the leg, centre hinge at the knee joint.
- Loosely fasten the two straps closest to the knee.
- Loosely fasten the remaining two straps.
- Pull straps tight to remove slack behind the leg. Be careful to maintain the lateral and medial positions of the hinge bars.
- Lock strap lock clips.
- Pull straps tight through the buckles. Be careful to maintain the lateral and medial positions of the hinge bars.
- Secure strap ends, use hook and loop Y-tabs at strap ends to affix straps. It may be necessary to shorten straps by folding them over before attaching Y-tabs.
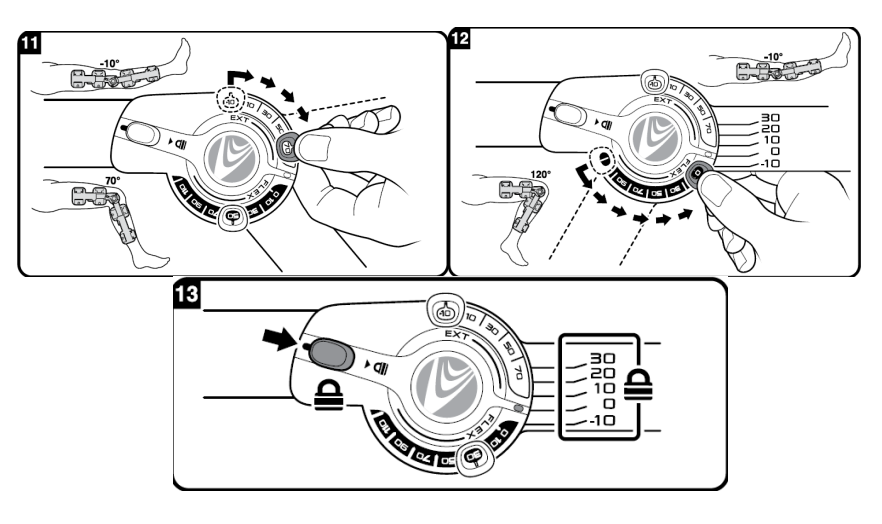
ROM (range of motion) hinge adjustment
- If you have been advised to change the settings of the ROM hinge on your knee brace, only do so at the indicated time frames and to the specified setting. The following will be explained to you at your first fitting appointment.
- Extension limit settings may be selected between -10° (Hyperextension) and 70° by pulling the tab out and sliding it to the desired position.
- Flexion limit settings may be selected between -10° and 120° (represented as last tick mark on scale).
- The hinge may be locked by sliding the quick lock button into the locked position at any one of 5 positions: -10° (hyperextension), 0° (Neutral), 10°, 20°, 30° of flexion.
Use and care of your knee ROM brace
After initial application, the brace may be removed and reapplied by unclipping the buckles only. You can hand wash the foam pads and straps with mild soap and air dry. Do not place pads or straps into a mechanical dryer. The following should be done to maintain good care of your supplied knee ROM brace:
- Brace should be worn underneath clothing directly on your skin to ensure the best fit and reduce slipping
- Check regularly for pressure areas from straps. Adjust straps as swelling fluctuates.
Can I walk in my brace?
Your clinician will instruct how much, and when, weight is to be put through your injured limb during your appointment. This may gradually increase over a period of time and be pain-dependant. No weight should be put through your limb if your brace has been removed (eg when washing or sleeping). Crutches may be necessary to provide balance when walking.
Can I remove my brace?
Your clinician will instruct the times at which you can remove your brace. This will include for washing, sleeping and to complete physiotherapy.
Exercises
It is important to exercise all joints not immobilised in your brace and to repeat every hour until fully functional. This helps to reduce swelling, stiffness, maintain some muscle strength and improve circulation. This can be painful and difficult to start with, but should improve within the first week.
- Wiggle your toes regularly
- Straighten and bend your knee (dependant on degree of ROM)
- Gently clench the muscles in the back of your calf and thigh to improve blood flow
- Move your hip.
Driving
Your insurance may not be valid whilst you are being treated with a knee brace. It should be stressed firmly that patients DO NOT drive whilst wearing a brace.
After your brace has been removed
Due to the long period of time that your limb has been immobilised, upon removal of your brace you may experience some of the following so do not panic:
- You may find that your leg feels thin and strange; this is normal
- You may experience swelling, discomfort and stiffness in the affected limb. This is quite normal and may continue for several weeks. You may find it helpful to keep the limb elevated
- Your skin may be dry and itchy. Do not scratch; try using baby oil or moisturiser
- Your skin will be sensitive. Be careful if going in the sun and apply a sun block
- Physical activities eg manual labour, sport etc should be reduced or avoided during the first few weeks after removal.
On the day of your follow-up appointment
You may require several treatments during your visit to clinic, such as x-rays and dressings. This, along with varying numbers of patients, means that sometimes you may have to wait longer than we would like, so we apologise for any inconvenience in advance.
DVT signs and symptoms
Due to immobilisation and reduced mobility, there is a higher risk of developing a DVT (deep vein thrombosis). It is important to stay as active as possible, drink plenty of fluids and be aware of the signs and symptoms.
Please contact the plaster room or the Emergency Department immediately if you experience any of the following:
- Pain in the calf, thigh or chest
- Sudden onset of shortness of breath with no physical exertion
- Swelling of the leg
- Increased or decreased warmth of the leg
- Redness in the leg
- Bluish skin discoloration.
Pressure ulcer
A pressure ulcer (sore) is a type of injury that breaks down the skin and underlying tissue. A small number of high risk patients are at increased risk of developing a pressure sore in a brace, which reduces mobility.
- Make sure to regularly reposition your leg throughout the day so that you are not constantly resting on the same area for long periods of time (every two hours)
- If you notice any discomfort or pain under the brace, most noticeably at the edges or heel, please contact the plaster room for urgent review
- Ensure the top and bottom of the brace is not rubbing and leaving red marks
- Do not rest the leg on the heel for long periods of time and place a pillow under the leg.
Further advice and instruction
To be completed by the orthopaedic team.
Contact us if you experience any of the following
- Your toes become painful, swollen or blue
- You are unable to move the limb/joints
- You feel ‘pins and needles’ or numbness in the limb
- Any ‘burning’, ‘blister-like’ pain or severe irritation under the boot
- Discharge, blood staining or wetness
- Excessive itching
Please contact the plaster room where a booked appointment can be made for you to return for assessment. Arriving without a prior appointment may result in longer waits or having to return at a convenient time. Outside of plaster room hours, please contact your local Minor Injuries Unit or the Emergency Department if urgent.
Contact numbers
We hope that you have found this information useful. If you have any questions or are worried about anything, please speak to the following Dorset County Hospital staff:
Orthopaedic Practitioners James Vincent, Sarah Nelmes and Zara Penwell
Plaster Room: 01305 255498
About this leaflet
Authors: James Vincent, Senior Orthopaedic Practitioner and Sarah Nelmes, Orthopaedic Practitioner
Written: April 2020
Approved: September 2020
Review date: September 2023
Edition: 1
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet