Coronary Artery Chronic Total Occlusion
What is a Chronic Total Occlusion (CTO)?
CTO is a type of heart disease where an artery becomes completely blocked for at least three months. This prevents blood from getting to the part of the heart supplied by that artery. Without enough blood flow, the heart does not receive the oxygen and nutrients it needs to function properly, resulting in angina.
Many patients with a CTO will develop an alternative circulation to the heart, which we refer to as collateral circulation; however, these collaterals may still not provide sufficient flow to the myocardium (heart muscle). CTOs are very common, occurring in as many as 30% of patients with coronary artery disease.
What are the treatment options?
As with any patient with stable coronary artery disease, secondary prevention medication is vital, as well as anti-anginal medication for symptom control.
Historically, patients who were found to have a CTO and were experiencing symptoms of angina (chest pain, shortness of breath, tiredness) despite maximum medical therapy, required open heart surgery – Coronary Artery Bypass Graft (CABG). Today, however, it is possible to treat CTO through a less invasive technique called Percutaneous Coronary Intervention (PCI). This procedure involves opening the artery using balloons and stents, and occasionally other specialist equipment. Your consultant cardiologist has recommended this as the next stage in management of your artery disease and your symptoms.
However, if you require more information regarding the alternative treatment options, please contact the Cardiology Department on 01305 255887.
CTOs are often heavily calcified and/or extremely fibrotic, therefore, the treatment of such lesions by PCI approach is considered highly challenging, with a success rate of 80-85%. It can often take two or more procedures to open the artery, so do not be disappointed if it
does not work first time. Often the first procedure creates tearing in the artery wall, which creates a new passage for the next attempt.
What are the benefits of CTO PCI?
Three possible benefits of CTO PCI are improvement in symptoms, improvement in left ventricular function (providing the myocardium is viable) and improvement in survival.
What to expect
You will be asked to attend a pre-assessment clinic prior to your procedure. At this appointment the nurse will be able to give you more details about the procedure, including preparation and aftercare.
On the day of the procedure you will be admitted to our day ward within the Cardiology Department where the nurse caring for you will undertake some pre-procedure checks, including blood pressure, ECG and insertion of a small tube into the vein in your arm. This is used during the procedure for any medication. CTO PCI can be a lengthy procedure, taking anything from one hour to three hours. Due to this you will be offered a temporary urinary catheter to make you more comfortable during the procedure, and also some sedation.
How is the CTO PCI performed?
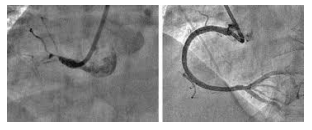
The procedure is similar to an Angiogram or Cardiac Catheterisation. You will lie on a narrow table in the catheterisation room. An X-ray camera is used to take pictures. CTO procedures are often carried out using two entry sites (both wrists, both groins or one wrist and one groin). This allows the doctor to position two catheters up to your heart so that the vessel can be visualised before and after the occlusion. A simultaneous injection of contrast into both the left and right coronary arteries is needed to show progress of the procedure. The blockage can then be targeted from the front and back (antegrade and retrograde).
Firstly, the Doctor will use a very fine wire in the coronary artery to create a passage through the blockage. Once this has taken place he can use balloon inflations and stent/s to widen the artery.
At the end of the procedure the leg artery is closed using an Angioseal (a dissolvable plug). If we cannot use an Angioseal, pressure will be used by a nurse, or a special pressure belt called a Femostop. If the wrist artery is used, a pressure band is placed around your wrist and will be kept on for two to three hours. You will then return to our ward area where the nurses will do regular checks on your blood pressure and wound site.
If the procedure has been relatively short and uncomplicated, you will be able to go home between four and six hours after the procedure, providing that you have someone to remain with you overnight. If the procedure is lengthy, or there have been complications, you will
be admitted to a cardiology ward for observation overnight.
What are the risks of the procedure?
- Bleeding – from the artery used for access (groin or wrist). This will be monitored closely by the nursing staff and treated by applying pressure
- Transient kidney damage – as a result of large volumes of contrast. The kidney function returns to normal within seven-14 days. Less than 1% of patients will require dialysis
- Heart attack can occur in less than one in 1000 cases
- Stroke can occur in less than one in 1000 cases
- Perforation – this is usually caused by the guidewire exiting the vessel. This can then lead to tamponade (a collection of blood around the heart), which can be treated by inserting a drain in through the centre of your chest. This happens in 2% of CTO cases.
- Radiation exposure – CTO procedures are often lengthy procedures resulting in radiation exposure that could lead to skin injury. This may not be apparent until weeks after the procedure and should be reported back to the cardiologist. You will be advised what to look out for if you have a high dose of radiation during your procedure
- Occasionally scar tissue forms inside the stent/s, which causes narrowing and causes your angina symptoms to return; this is call ‘restenosis’. This is rare and can be treated. There is a small risk of a blood clot forming which could block the stent/s. To avoid this please continue taking your anti-platelet medication (Clopidogrel/Ticagrelor) for 12 months after the procedure, unless told otherwise by the cardiologist.
What happens after the procedure?
- You must have someone at home for the first 24 hours following the procedure if you are discharged the same day
- You will be expected to refrain from any physical activity for the first week
- You must not drive for one week following the procedure. This is the DVLA rules
- Your Doctor will advise you when to return to work
- Arrangements will be made for you to be followed up by the cardiac rehab nurses four weeks after the procedure.
Further information
You will be invited to a pre-assessment appointment where the nurses will be able to answer any further questions. If there is anything urgent, you can contact the Cardiology Department on 01305 255887.
About this leaflet
Author: Laura Starr, Senior Sister Cardiology Department
Written: December 2016
Updated and approved: November 2021, February 2025
Review date: February 2028
Edition: v2
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet