Trabeculectomy Surgery
This leaflet provides information about trabeculectomy surgery to treat glaucoma. It will help you to understand the procedure, its risks and benefits, and the care that you will receive. If you would like additional information about glaucoma and what the surgery involves,
please speak to one of the doctors or nurses. They will be more than happy to help.
What is glaucoma?
Glaucoma is a condition which affects the nerve (optic nerve) at the back of your eye which is like a cable connecting your eye to the brain. In glaucoma, this nerve undergoes progressive damage which leads to loss of sight. Initially, glaucoma causes loss of your ‘peripheral vision’ before it involves your ‘central vision’ in the very advanced stages. There are many risk factors for glaucoma, but increased pressure inside your eye (intra-ocular pressure or IOP) is the most commonly implicated and the only treatable risk factor for this condition. By reducing your IOP, glaucoma progression can be halted, and sight loss can be prevented. Any loss of vision which has already occurred due to glaucoma however,
cannot be restored by treatment. A small number of people’s glaucoma may continue to progress or worsen despite lowering the IOP.
Why have you been advised to have glaucoma surgery and what are its benefits?
Initially, your eye doctor would have prescribed drops, laser treatment or both to reduce the IOP. In some people with glaucoma, the condition continues to worsen despite this, meaning the IOP needs to be reduced further. This can only be achieved with the help of glaucoma surgery. In some people with very advanced glaucoma, the eye doctor might advise surgery straightaway without trialling the eye drops or laser treatment. This surgery aims to reduce the IOP down to a minimum so that your eyesight can be preserved. Any vision lost, cannot be recovered with surgery.
The most obvious benefit is to preserve sight and prevent further loss of vision from glaucoma
What happens in trabeculectomy surgery?
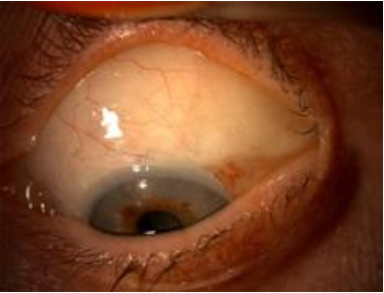
Trabeculectomy surgery aims to create a new drainage channel in your eye allowing fluid from within your eye to easily escape into a ‘filtering bleb’ which is hidden underneath your upper eyelid. This will not usually affect the appearance of your eyes. An anti-scarring agent (Mitomycin C) is also applied at the same time to prevent future scarring. If surgery is successful, you will have this ‘bleb’ and the effects of it for life.
How successful is the operation?
The success of this surgery depends on many factors including the type of glaucoma, duration of using anti-glaucoma drops, age, ethnicity, previous eye surgery and general health conditions.
However, studies have demonstrated an overall success rate of 70 to 80%. That means seven to eight out of 10 people will have adequately reduced IOP without added anti-glaucoma drops. However, 10-20% will need to restart the anti-glaucoma drops to keep the pressures under control.
What are the possible risks of trabeculectomy?
There are always risks associated with any procedure. As far as trabeculectomy is concerned, complications can happen at any time during or after the operation. The two most serious risks which can result in sight loss are:
- Bleeding inside the eye called a ‘suprachoroidal haemorrhage’
- A serious infection inside the eye called ‘endophthalmitis’ which remains a lifetime risk after the operation.
Fortunately, these two complications are very rare and occur in less than one in 1000 patients.
The other frequently occurring but less serious risks are:
- Very low or high pressures. Additional treatments may be advised by your eye doctor if this happens such as tablets, drops, laser or removing sutures from the eye and occasionally a revision operation is necessary
- Bleeding within the eye (called hyphaema) which generally resolves by itself
- Reduced vision. Up to 30% of patients may experience slightly reduced vision after trabeculectomy. This can be because of a change in prescription which may be corrected with updated glasses. It can also be because of a developing cataract which frequently progresses after glaucoma surgery. Cataract surgery may be indicated later, if needed
- Scarring of the filtration bleb. It is your body’s natural response to surgery which leads to scarring of the bleb and the filtration from the eye slows down, leading to a build-up of the eye pressure. This is generally treated by either continued steroid drops or sometimes your eye doctor may recommend an additional procedure called ‘bleb needling’ to release the scar tissue. Sometimes the scar tissue can be quite thick and can lead to failure of the procedure. In such cases, your eye doctor may need to ‘re-do’ or ‘revise’ the original surgery or recommend a glaucoma drainage device placement
- Inflammation within the eye, which can be treated with eye drops
- Infection within the ‘bleb’ called ‘blebitis’ and would need intensive antibiotic treatments. This happens in less than five in 100,000 patients
- Ocular irritation, especially in patients who suffer from dry eyes
- A few patients may feel the bleb underneath their eyelid and occasionally get discomfort called ‘bleb dysesthesia’. Lubricating eye drops helps relieve the symptoms. This condition sometimes persists and requires a bleb revision operation
- Droopy eyelid on the operated side occurs in 10-20% of patients. This may be very mild or may be significant enough to require eyelid surgery to lift it up
- Mild double vision is common which settles down in within a few weeks. Very rarely, double vision can be persistent, which may require treatment. The treatment depends upon the cause and the severity of double vision and may require adjustment in your glasses prescription to correct new astigmatism, prisms in your glasses or surgery on muscles which control eye movements
- Very rarely, clouding of the cornea occurs which affects vision
- The complications in the retina are very rare, such as swelling at the back of the eye (macular oedema) which can be treated with steroid drops, and retinal detachment which will need to be surgically repaired. This requires a referral to a vitreo-retinal surgeon.
What do I have to do before the operation?
You must continue your anti-glaucoma eye drops or tablets as usual up to the day of the surgery. Surgeon may adjust your eye drops to help reduce the inflammation of the eye and may prescribe a short course of anti-inflammatory eye drops before the operation. You will be asked to attend a pre-operative assessment and please bring an up-to-date prescription which includes all your current medications. Please inform the nurse if you are on any blood thinners.
On the day of surgery
The surgery is generally performed under local anaesthesia. An injection to numb your eye will be given and you will be awake during the procedure. Sometimes your eye doctor may prescribe a sedative tablet to calm you down if you are feeling anxious. Please do not wear
any eye make-up on the day of surgery and wear comfortable clothes. The operation will be performed by a senior consultant experienced in glaucoma surgery or will be performed by a junior surgeon in training under supervision. Occasionally, general anaesthesia will be
offered, if indicated.
What happens after the surgery?
Your eye will be red or bloodshot and slightly sore after the operation which may last for a few days to a week. It is normal for your eyes to feel slightly sticky and gritty after the operation. You may notice slight blood in your tears which is very common and settles down within few hours. You will be asked to stop the anti-glaucoma drops in the operated eye but should continue to use them in the other eye. A separate set of drops will be given to use in the operated eye for a period of two to three months.
What activities can I do after the surgery?
You should avoid any strenuous activity after the operation such as going to the gym, playing sports or swimming for at least 3 months after the operation. However, you can watch TV, read, or go out for leisurely walks after the operation. There are no restrictions on flying. Driving will depend on your vision and degree of glaucoma, which will be discussed with your eye doctor.
Follow-up visits
Your eye doctor will want to see you the next day after the operation, and then every two to four weeks for a period of two to three months, depending on the pressure and how you are settling after the operation. Your eye drops may be altered by your doctor on every visit.
In case of emergency
Please get in touch immediately if you experience:
- Severe pain in the eye
- Increasing redness
- Increased loss of vision.
You can contact the eye clinic casualty triage on 01305 255192 or attend the Emergency Department.
Useful websites
About this leaflet
Authors: ST Dr Priyadarshini Suresh and Consultant Ophthalmologist Mr Usama Faridi
Written: March 2024
Approved: May 2024
Review Date: May 2027
Edition: v1
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet